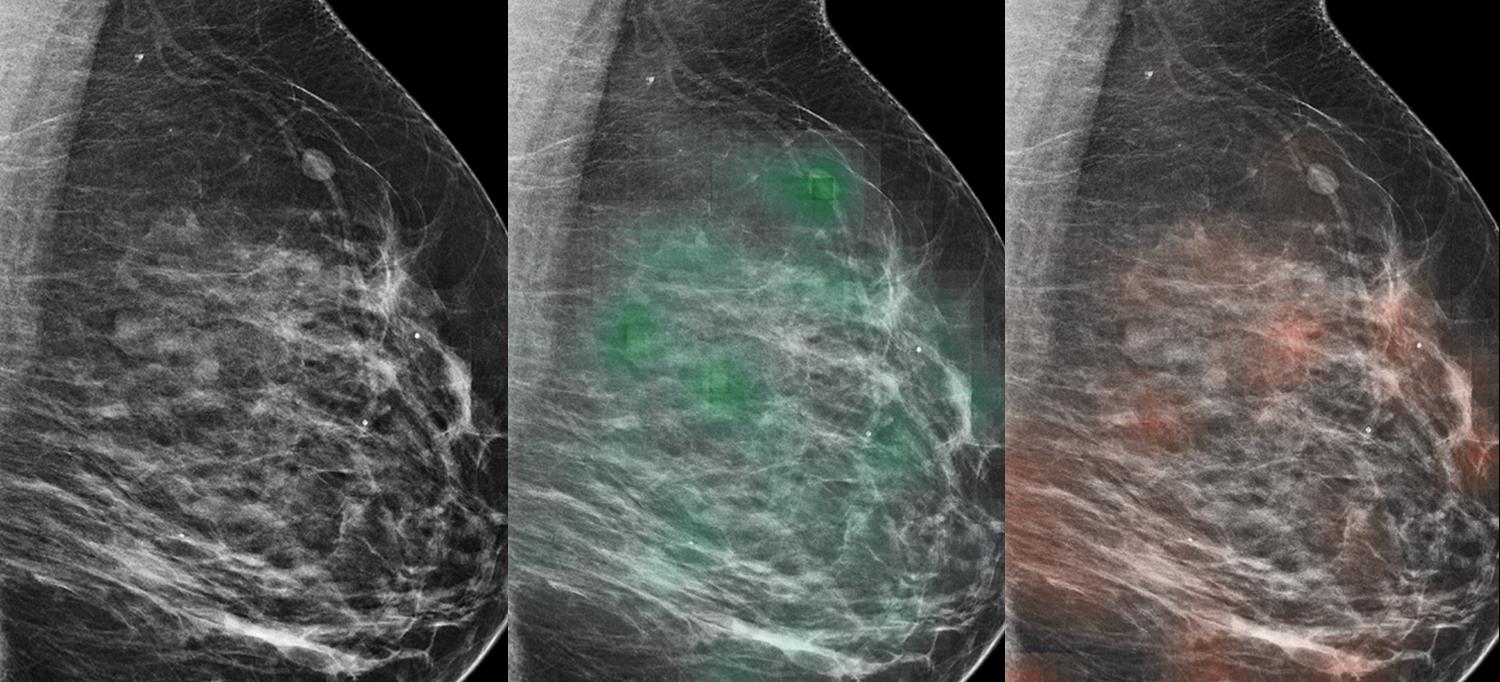
An AI tool learned to predict which lesions were likely malignant (red heat map) or likely benign (green heat map), with potential to aid radiologists in the diagnosis of breast cancer.
Images courtesy of NYU School of Medicine
An artificial intelligence (AI) tool—trained on roughly a million screening mammography images—identified breast cancer with approximately 90 percent accuracy when combined with analysis by radiologists, a new study finds.
Led by researchers from NYU School of Medicine and the NYU Center for Data Science, the study examined the ability of a type of AI, a machine learning computer program, to add value to the diagnoses reached by a group of 14 radiologists as they reviewed 720 mammogram images.
“Our study found that AI identified cancer-related patterns in the data that radiologists could not, and vice versa,” says senior study author Krzysztof J. Geras, PhD, assistant professor in the Department of Radiology at NYU Langone.
“AI detected pixel-level changes in tissue invisible to the human eye, while humans used forms of reasoning not available to AI,” adds Dr. Geras, also an affiliated faculty member at the NYU Center for Data Science. “The ultimate goal of our work is to augment, not replace, human radiologists.”
In 2014, more than 39 million mammography exams were performed in the United States to screen women (without symptoms) for breast cancer and determine those in need of closer follow-up. Women whose test results yield abnormal mammography findings are referred for biopsy, a procedure that removes a small sample of breast tissue for laboratory testing.
A New Tool to Identify Breast Cancer
In the new study, the research team designed statistical techniques that let their program “learn” how to get better at a task without being told exactly how. Such programs build mathematical models that enable decision-making based on data examples fed into them, with the program getting “smarter” as it reviews more and more data.
Modern AI approaches, inspired by the human brain, use complex circuits to process information in layers, with each step feeding information into the next, and assigning more or less importance to each piece of information along the way.
Published online recently by the journal IEEE Transactions on Medical Imaging, the current study authors trained their AI tool on many images matched with the results of biopsies performed in the past. Their goal was to enable the tool to help radiologists reduce the number biopsies needed moving forward. This can only be achieved, says Dr. Geras, by increasing the confidence that physicians have in the accuracy of assessments made for screening exams (for example, reducing false-positive and false-negative results).
For the current study, the research team analyzed images that had been collected as part of routine clinical care at NYU Langone Health over seven years, sifting through the collected data and connecting the images with biopsy results. This effort created an extraordinarily large dataset for their AI tool to train on, say the authors, consisting of 229,426 digital screening mammography exams and 1,001,093 images. Most databases used in studies to date have been limited to 10,000 images or fewer.
Thus, the researchers trained their neural network by programming it to analyze images from the database for which cancer diagnoses had already been determined. This meant that researchers knew the “truth” for each mammography image (cancer or not) as they tested the tool’s accuracy, while the tool had to guess. Accuracy was measured in the frequency of correct predictions.
In addition, the researchers designed the study AI model to first consider very small patches of the full resolution image separately to create a heat map, a statistical picture of disease likelihood. Then the program considers the entire breast for structural features linked to cancer, paying closer attention to the areas flagged in the pixel-level heat map.
Rather than have the researchers identify image features for their AI to search for, the tool is discovering on its own which image features increase prediction accuracy. Moving forward, the team plans to further increase this accuracy by training the AI program on more data, perhaps even identifying changes in breast tissue that are not yet cancerous but have the potential to be.
“The transition to AI support in diagnostic radiology should proceed like the adoption of self-driving cars—slowly and carefully, building trust, and improving systems along the way with a focus on safety,” says first author Nan Wu, a doctoral candidate at the NYU Center for Data Science.
Along with Dr. Geras, study authors from the Department of Radiology at NYU Langone were Eric Kim, Stacey Wolfson, Ujas Parikh, Sushma Gaddam, Leng Young Lin, Joshua Weinstein, Krystal Airola, Eralda Mema, Stephanie H. Chung, Esther Hwang, Naziya Samreen, Beatriu Reig, Yiming Gao, Hildegard B. Toth, Kristine M. Pysarenko, Alana A. Lewin, Jiyon Lee, S. Gene Kim, Laura Heacock, and Linda Moy. Authors from the NYU Center for Data Science were Nan Wu, Jason Phang, Jungkyu Park, Yiqiu Shen, Zhe Huang, Thibault Févry, and Kyunghyun Cho, who is also on the faculty of NYU Courant Institute of Mathematical Sciences. Other authors were Kara Ho at SUNY Downstate College of Medicine; Masha Zorin in the Department of Computer Science and Technology at the University of Cambridge; Stanisław Jastrzębski from Jagiellonian University; and Joe Katsnelson in the Department of Information Technology at NYU Langone.
This work was supported in part by National Institutes of Health grants R21CA225175 and P41EB017183. The model used in this study has been made available to the field to drive innovation.
Media Inquiries
Greg Williams
Phone: 212-404-3500
gregory.williams@nyulangone.org

