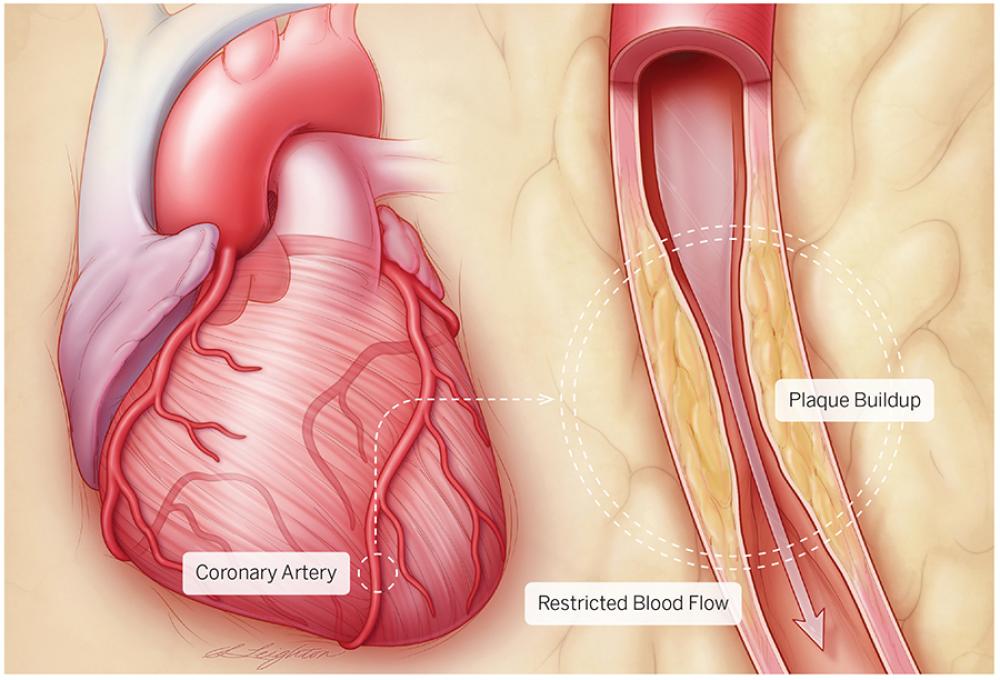
Each year, some 735,000 Americans suffer a heart attack, often with little warning. About one-third of these people die, and those who survive often have permanently weakened heart muscles. Although heart attacks may seem to strike out of the blue, they are most often the result of coronary artery disease, or CAD, a gradual, toxic process of plaque accumulation in arteries, occuring over decades. The good news is that most heart attacks are preventable with the right interventions and treatments, according to cardiologists at the Center for the Prevention of Cardiovascular Disease within the Leon H. Charney Division of Cardiology at NYU Langone.
The center cares for people who are at high risk for developing cardiovascular disease, as well as those who have already experienced a heart attack or stroke, or have had heart surgery, vascular surgery, or angioplasty. Its team includes some of NYU Langone’s leading cardiologists. “We’ve achieved excellent success using state-of-the-art diagnosis and medications along with lifestyle modifications,” says the center’s director, Edward Fisher, MD, PhD, the Leon H. Charney Professor of Cardiovascular Medicine, who has conducted pioneering research on the biology of cardiovascular disease. “We’ve staved off heart attacks in most of the patients we’ve treated.”
These four strategies are key to their success.
1. Assess Risk
The buildup of a waxy substance containing cholesterol that forms plaques in the heart’s three large coronary arteries—coronary artery disease—sets the stage for a potential heart attack. Even small plaques may rupture, causing a blood clot that blocks blood flow to your heart, which is how most heart attacks occur. Unless the blockage is treated immediately, the result can be permanent damage to the heart or even death. The key to preventing a heart attack is to halt plaque formation by bringing risk factors for CAD under control. “Our center spends a lot of time assessing risk,” explains cardiologist Arthur Schwartzbard, MD. Traditional risk factors include high blood pressure; high LDL, or “bad” cholesterol; low HDL, or “good” cholesterol; diabetes; smoking; and age. The more risk factors you have, the higher your risk for CAD. “Each risk factor has an additive effect on the others,” says Howard Weintraub, MD, the center’s co–clinical director.
2. Get the Right Tests
Most people get basic lipid, blood pressure, and glucose screens with their annual physical. Dr. Weintraub suggests an additional screen for the total number of LDL particles, which may be particularly useful in patients with higher levels of triglycerides. He also advises testing for lipoprotein LP(a), a particle that adds significantly to CAD risk and is not routinely measured. The experts stress the importance of addressing these risk factors earlier and more aggressively if you have a parent or sibling who developed CAD before age 50.
3. Address Every Risk Factor
Once a patient’s risk status is fully assessed, the team presses on all fronts. As needed, they’ll use blood pressure medication to maintain healthy blood pressure, and prescribe diabetes medications plus weight loss and exercise to keep blood glucose in normal ranges. They may also prescribe antiplatelet medications (including low-dose aspirin) to prevent blood clots.
The center’s most intensive focus, however, is on lowering LDL cholesterol—the primary source of arterial plaque lipid. Your body makes most of the LDL in your bloodstream. This production can be reduced by cutting intake of saturated animal fats—which the body eventually turns into LDL cholesterol—as well as increasing dietary fiber and taking medications that spur the removal of LDL from the blood.
The first-line treatment is usually a cholesterol-lowering statin medication. For people who have difficulty tolerating statins, the center has pioneered an approach in which long-acting statins are taken every two or three days. For patients who can’t tolerate statins at all, the center’s director of integrative medicine, cardiologist Dennis Goodman, MD, offers natural alternatives.
4. Encourage a Healthy Diet and Exercise
The center’s cardiologists are not only experts at medical management of CAD, but also passionate proponents of a healthy diet and daily exercise. “Research shows that the best preventive diets include a high intake of vegetables, fruits, whole grains, and fiber, and low intake of animal and dairy fat, sugar, and processed carbohydrates,” explains cardiologist Eugenia Gianos, MD. These include the Mediterranean diet, vegan diets, and the DASH diet, short for Dietary Approaches to Stop Hypertension.
A recent large-population study in Spain found that the Mediterranean diet lowered risk of coronary events by 30%—as much as medications. Evidence also shows that just 30 minutes of aerobic exercise daily significantly reduces risk. “Any activity that raises your heart rate will work,” explains Dr. Fisher, “including brisk walking.”