The endometrium-free closure technique used for cesarean deliveries aims to minimize uterine scar defects and improve outcomes for mothers.
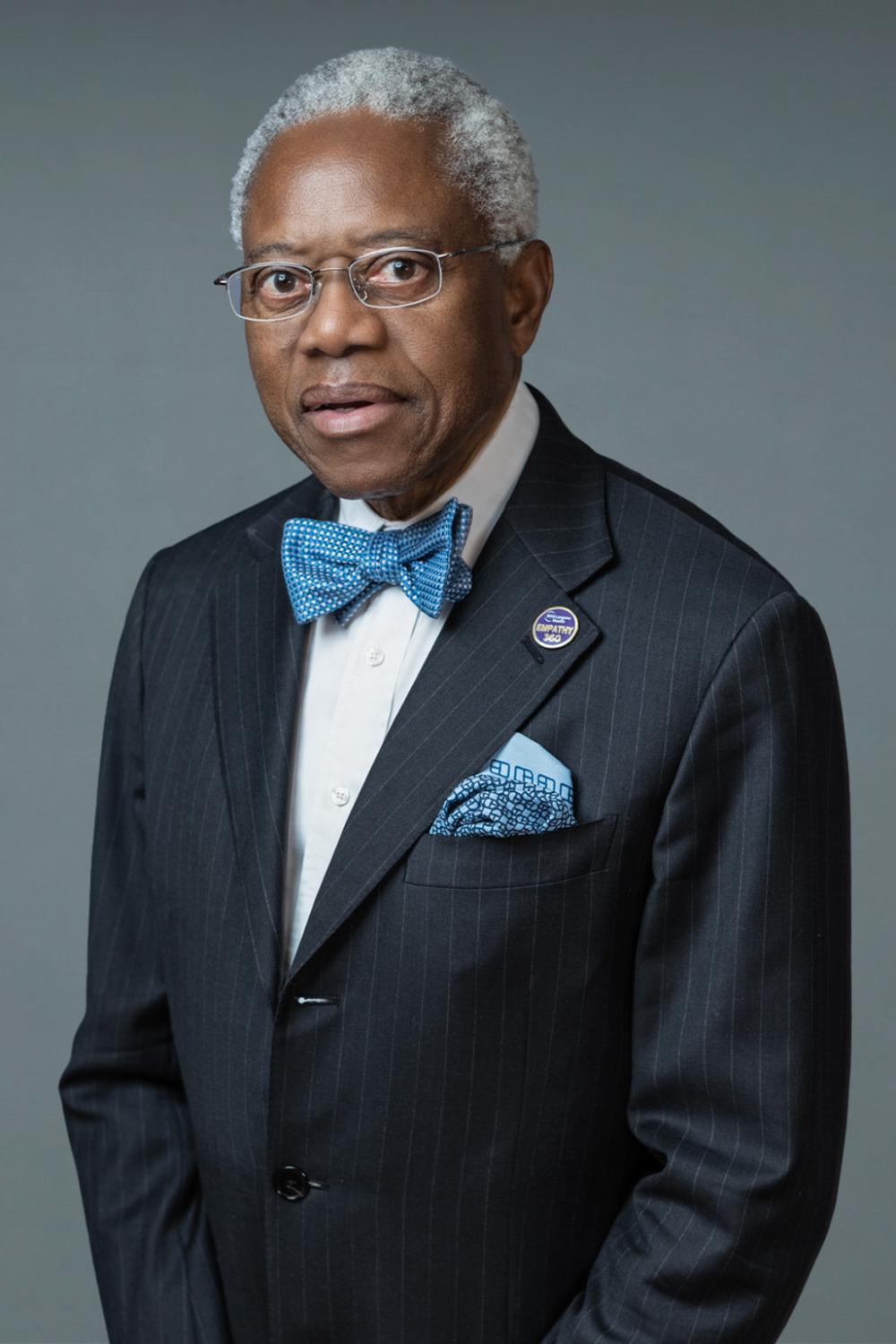
Credit: Getty / Vesnaandjic
As cesarean delivery (C-section) rates continue to rise worldwide, experts at NYU Langone Health are highlighting a surgical technique that may help lower the risk of long-term complications. The endometrium-free closure technique (EFCT), described in a new article published online in the American Journal of Obstetrics & Gynecology, focuses on how the uterus is closed after a cesarean delivery to support better healing.
After a cesarean delivery, some patients develop small pockets or dents in the scar where the uterus was opened. These scar defects can cause symptoms like irregular bleeding, pelvic pain, or infertility. In some cases, they can also increase the risk of complications in future pregnancies, including placenta accreta spectrum.
“Even small refinements in surgical technique can have meaningful impacts on reproductive health,” said Clarel Antoine, MD, clinical professor in the Department of Obstetrics and Gynecology at NYU Grossman School of Medicine. “By avoiding the inner lining of the uterus during the repair, we can reduce scar defect formation and lower the risk of problems in future pregnancies.”
In many common closure approaches, the inner lining of the uterus is included in the stitches used to close the incision, which research suggests may interfere with healing. With EFCT, surgeons carefully identify this lining and avoid stitching through it.
Previous studies have shown fewer and smaller scar defects when this lining is not included in the closure, as well as thicker, healthier tissue where the uterus was repaired. Although previous research has compared different closure styles, this paper points out that precision and correct alignment of the uterine layers appear to matter most.
“As C-section rates continue to increase worldwide, evidence-based refinements in technique are critical,” said Dana R. Gossett, MD, the Stanley H. Kaplan Professor and Chair of Obstetrics and Gynecology. “This approach has potential to improve long-term reproductive outcomes and future studies should be conducted to assess its impact.”
Dr. Antoine and study co-authors note that further randomized trials are needed, particularly in complex or emergency cases where the uterus may be harder to visualize. They emphasize the importance of training surgeons to recognize the different layers of the uterus so they can be repaired correctly.
About NYU Langone Health
NYU Langone Health is a fully integrated health system that consistently achieves the best patient outcomes through a rigorous focus on quality that has resulted in some of the lowest mortality rates in the nation. Vizient, Inc., has ranked NYU Langone No. 1 out of 118 comprehensive academic medical centers across the nation for four years in a row, and U.S. News & World Report recently ranked four of its clinical specialties No. 1 in the nation. NYU Langone offers a comprehensive range of medical services with one high standard of care across seven inpatient locations, its Perlmutter Cancer Center, and more than 320 outpatient locations in the New York area and Florida. The system also includes two tuition-free medical schools, in Manhattan and on Long Island, and a vast research enterprise.
Media Inquiries
Lacy Scarmana
Phone: 646-754-7367
Lacy.Scarmana@NYULangone.org