Photo: digicomphoto/Getty
A 52-year-old woman presented to the emergency department (ED) at NYU Langone Hospital—Brooklyn complaining of acute-onset middle back pain that started 3 days prior. She described the pain as sharp and radiating to her neck, rated the intensity as 8 on a scale of 1 to 10, and stated that it worsened with deep inspiration or other movements.
Three weeks before her ED visit, the patient had experienced sinus pain, a cough, and a low-grade fever. She tested positive for coronavirus disease (COVID-19) and self-quarantined. Her medical history included a diagnosis of scleromyxedema (SM). The condition causes papular and sclerodermoid eruption in the setting of monoclonal gammopathy of undetermined significance (MGUS; see Koronowska et al., 2013, and Baxi et al., 2019). The patient had also been diagnosed with Hashimoto’s disease and asthma, and had been receiving intravenous immunoglobulin (IVIG) for the past seven years. In the ED, however, she did not present with associated symptoms such as fever, chills, shortness of breath, chest pain, abdominal pain, or headache.
Resolving the diagnosis and initiating an effective intervention required careful coordination among ED, hospital medicine, and rheumatology providers, including Yamen Homsi, MD, MPH, at NYU Langone Health. In the ED the patient was alert and oriented, and her vitals were normal with the exception of an elevated 154/94 blood pressure reading and heart rate of 90. Her heart, lung, abdomen, and extremities exams were all normal, with no rash, skin tightness, or lymphadenopathy. An initial electrocardiogram (EKG) and chest X-ray were both unremarkable.
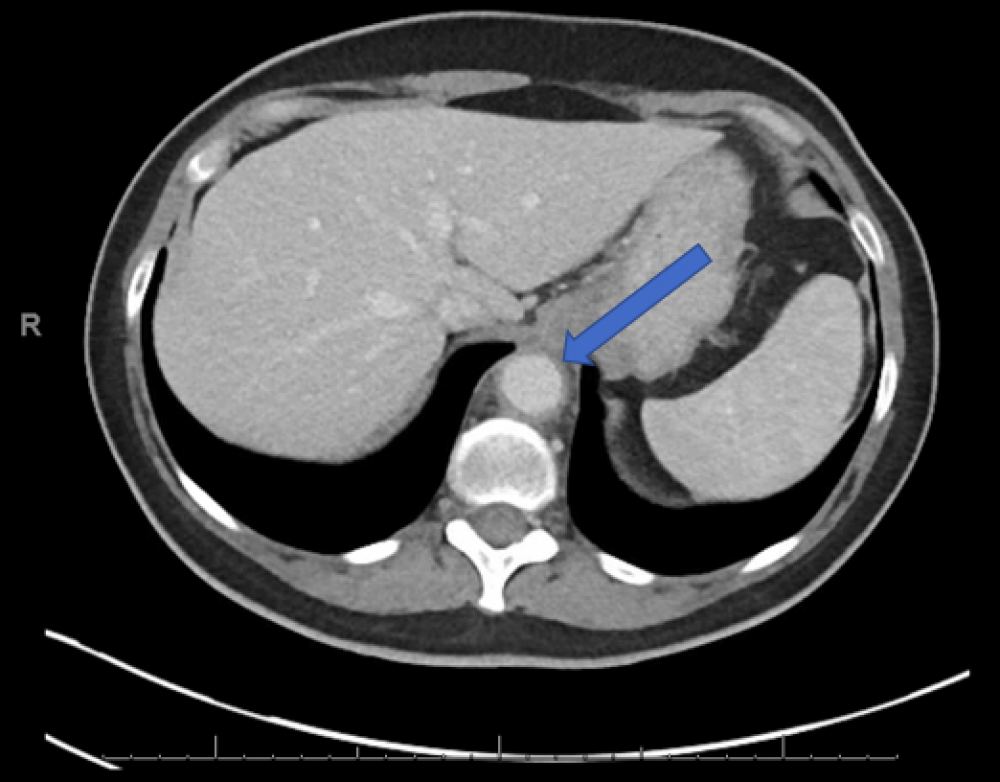
Likewise, the patient had a normal complete blood count and C-reactive protein levels, but an abnormally high erythrocyte sedimentation rate (ESR) of 120 mm per hour, indicating inflammation. The ED team performed a chest CT with IV contrast, which was negative for pulmonary embolism but showed distal aortic stranding, a concerning sign of aortitis. Subsequently, the patient underwent an abdominal CT with contrast that revealed wall thickening and perivascular stranding of the distal thoracic aorta extending inferiorly to the level of the origin of celiac axis, a finding consistent with segmental aortitis.
Multiple noninfectious and infectious etiologies for aortitis have been described (see Gornik and Creager, 2008), and we ruled out many of them through extensive lab tests, including negative tests for syphilis, tuberculosis, hepatitis B, and hepatitis C, as well as a normal urinalysis. The patient’s antinuclear antibody (ANA) test titer of 1:160 showed a homogenous pattern. She tested positive for SS-A/Ro antibodies and borderline positive for anti-RNP and anti-CCP antibodies, but negative for rheumatoid factor, anti-dsDNA, anti-Smith, and anti-SSB antibodies.
After starting the patient on high-dose (500 mg per day) intravenous methylprednisolone for 3 days, she was switched to oral prednisone (60 mg per day), and her back pain resolved during the hospitalization. Methotrexate was added to her treatment regimen, and she was successfully tapered off prednisone. A repeat abdomen/chest CT three months later showed that her aortitis had completely resolved; her ESR had also normalized. The patient continues to receive methotrexate, as well as IVIG for her SM, without any signs of relapse.
Beyond established etiologies of aortitis, doctors have recently reported large vessel vasculitis after infection with SARS-CoV-2, while others have linked systemic vascular dysfunction and endothelial cell injury in the setting of an aberrant cytokine response to the viral infection (see Oda et al., 2020, and McGonagle et al., 2021). In fact, clinicians have described multiple vasculitic phenomena such as cutaneous vasculitis, Kawasaki-like disease spectrum, and pauci-immune thrombogenic vasculopathy in association with COVID-19 (see McGonagle et al., 2021). As probable explanations for such phenomena, they have proposed factors such as direct viral endotheliitis, complement-mediated vascular injury, and autoimmunity.
Because the patient developed aortitis very shortly after her COVID-19 infection, a hyperinflammatory state triggered by SARS-CoV-2 was believed to be behind her acute condition. Aortitis continues to be a challenging clinical diagnosis, and this complex case reaffirms that multidisciplinary collaboration, high suspicion, and proper workup to reveal underlying causes are essential for guiding the correct treatment.
References
Baxi KD … Jagati A. Monoclonal gammopathy of undetermined significance-associated scleromyxoedema. Indian Dermatol Online J. 2019. PMCID.
Gornik HL and Creager MA. Aortitis. Circulation. 2008. DOI.
Koronowska SK … Żaba R. Scleromyxedema: A rare disorder and its treatment difficulties. Postępy Dermatol Alergol. 2013. DOI.
McGonagle D … Watad A. COVID-19 vasculitis and novel vasculitis mimics. Lancet Rheumatol. 2021. DOI.
Oda R … Ohmagari N. Case of adult large vessel vasculitis after SARS-CoV-2 infection. Ann Rheum Dis. 2020. DOI.