Photo: NYU Langone Staff
An internationally recognized authority in developmental therapeutics and skin cancers, Janice Mehnert, MD, joined NYU Langone Health’s Perlmutter Cancer Center in July 2020 as associate director for clinical research. Dr. Mehnert, professor in the Department of Medicine, was previously an associate professor of medicine at Rutgers Robert Wood Johnson Medical School, where she was recruited in 2007 to develop a clinical and translational research program for the expert diagnosis and treatment of skin cancers.
At Perlmutter Cancer Center, Dr. Mehnert sees people with melanoma and other skin cancers and conducts multiple types of industry and cooperative group trials as well as investigator-initiated studies. She also is working to expand early phase trial activity in collaboration with the cancer center’s network sites in Brooklyn at Perlmutter Cancer Center—Sunset Park and on Long Island at Perlmutter Cancer Center at NYU Langone Hospital—Long Island, and further develop a strong culture of clinical and translational investigation.
She discusses her role as associate director for clinical research, what led her to join Perlmutter Cancer Center, and more.
Tell us about your role as associate director for clinical research and your goals for Perlmutter Cancer Center’s Clinical Trials Office.
My role is to ensure that we have resources running smoothly to provide support for the clinical research we do across all of our Disease Management Groups at Perlmutter Cancer Center. I also help align our investigator-initiated research with our scientific priorities, meaning the science that comes out of the Perlmutter Cancer Center research program. My role also includes strategic planning for expanding our clinical research footprint at our network campuses in Brooklyn and on Long Island and expanding our clinical research in collaboration with the National Cancer Institute. I am also committed to developing our infrastructure to mentor and grow junior faculty. Clinical investigation is a challenging path; I hope to be a voice of support and change for those who have selected this space for their life’s work.
An important objective is increased access to clinical trials for the significant populations of patients that Perlmutter Cancer Center reaches on campuses that are not our main campus in Manhattan. Identifying the types of research that can be done at a location close to the patient’s home whenever possible, because cancer often doesn’t travel well, and improving the patient experience are very important to us. We also want to identify and communicate the select opportunities for when patients must be referred into the Manhattan campus to receive essentially groundbreaking cancer care, since there are times when a specific procedure or clinical trial may only be accessed here.
Can you tell us about your work at the Rutgers Cancer Institute and what led you to join Perlmutter Cancer Center?
I spent a lot of my career at Rutgers. Part of the reason I was so proud to work at Rutgers was that, at the time, it was the only NCI-designated cancer center in the state of New Jersey. Without folks like me and my colleagues doing that kind of work, those patients would not have access to clinical trials. The same mission applies at Perlmutter Cancer Center. There’s an institutional mission to reach the patient and to reach the patient with clinical research, and that’s now expanding past Manhattan out into Brooklyn and Long Island. Because I had already done that at my home center at Rutgers, the prospect of doing that kind of work on a much larger scale was very exciting. Plus, I trained in Manhattan (internal medicine, The Mount Sinai Hospital), and there truly is no place like New York City when it comes to incredible innovation, energy, and people.
Also, I got to know the leadership team at Perlmutter Cancer Center (Benjamin G. Neel, MD, PhD, director of Perlmutter Cancer Center, Kwok-Kin Wong, MD, PhD, director of the Division of Hematology and Medical Oncology, and Jeffrey S. Weber, MD, PhD, deputy director of Perlmutter Cancer Center) when we worked together to submit a large multi-institutional grant. I began to see what was happening at Perlmutter Cancer Center from afar and recognized the absolutely tremendous growth that was happening in a relatively short period of time. I visited the campus for the first time in January 2019 and left amazed. That, coupled with the extremely strong science at Perlmutter Cancer Center and an institutional mission to put the patient experience front and center with respect to clinical research—which is something that I am really passionate about—were all very important things to me.
Now that you have been at Perlmutter Cancer Center for several months, what strikes you about the culture here?
I like that the faculty and staff really are invested in coming to work, rolling up their sleeves, and trying to do something about cancer. That’s been a delight. Even in the middle of a pandemic where it’s hard to meet individual people, it’s still been a very, very enjoyable experience. As I mentioned, the science is top-notch, and the number of people I can interact with in a given week working on so many different facets of cancer biology or immunology is quite significant. That part has been quite wonderful as well.
What should people with cancer know about clinical trials at Perlmutter Cancer Center and the outlook for cancer treatment in general?
Our Phase 1 Drug Development Program is a space to watch because we have growing strengths in genomics and immunology. And the contributions we are making to both precision oncology and precision immunology are my favorite spaces to watch at the moment.
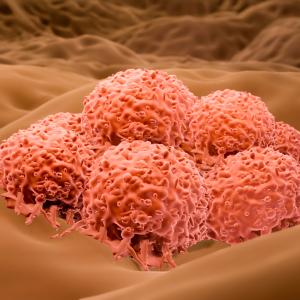
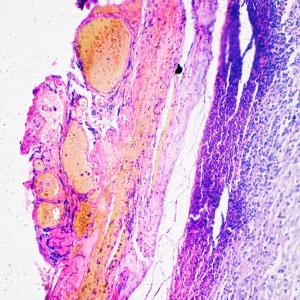
We are looking at genomically directed strategies, in which we identify, based on the characteristics of a tumor, the right way to treat the cancer. Immunotherapy is more complicated because the immune system is very dynamic, and finding just one marker that is going to predict immune response is a lot trickier, but we’re trying to do that. We’re looking at serum autoantibody profiles to predict toxicity. We are looking at dynamic measurements of how the immune system is at play within tumors, which ultimately means choosing the ideal strategy to fight somebody’s cancer.