Late-breaking developments in an mRNA cancer vaccine were among the presentations covered.
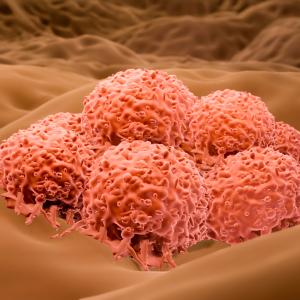
Credit: JaySi/Getty
Researchers from NYU Langone Health’s Perlmutter Cancer Center are presenting their latest findings and research at the 2024 American Society of Clinical Oncology (ASCO) Annual Conference, held May 31 to June 4 at Chicago’s McCormick Place.
Among these presentations:
- a three-year update on the long-term efficacy of an mRNA vaccine for use in patients being treated for metastatic melanoma
- a retrospective look at treatment patterns and outcomes in patients with advanced endometrial cancer
- a look at the safety and efficacy of a noninvasive combination treatment for patients with recurrent glioblastoma
“This year’s crop of presentations is a showcase of the Perlmutter Cancer Center’s commitment to delivering the highest level of research and clinical care,” said Alec Kimmelman, MD, PhD, the center’s director.
Late-Breaker Rapid Oral Abstract: Three-year update on the long-term efficacy of an mRNA vaccine for use in patients being treated for metastatic melanoma
Monday, June 3, 10:15AM CT
In a follow-up presentation at ASCO to the recently published clinical trial describing the effectiveness of combining the immunotherapy drug pembrolizumab with V940—an investigational individualized neoantigen mRNA vaccine for people with high-risk, surgically removed melanoma —this three-year update looks at the longer-term recurrence rates of treated patients.
The primary analysis of the phase 2 trial, led by Jeffrey S. Weber, MD, PhD, deputy director of Perlmutter Cancer Center, and sponsored by Moderna and Merck, assessed patients who received the vaccine, called mRNA-4157/V940, and the immunotherapy drug pembrolizumab, comparing their risk of recurrence and development of distant metastases to those who had received only pembrolizumab.
This three-year follow-up analysis showed a higher percentage of durable and meaningful long-term recurrence-free survival or survival without distant spread of cancer in patients who received both treatments (74.8 percent) compared to those who received only pembrolizumab (55.6 percent). The patients’ overall survival also improved with combination treatment, at 96.0 percent compared to 90.2 percent with pembrolizumab alone.
“This additional information continues to support the potential of mRNA-4156/V940 in combination with pembrolizumab for patients with metastatic melanoma,” said Dr. Weber. “We have followed up this work with a randomized phase 3 trial in more than a thousand patients, which we hope will provide a definitive assessment of the efficacy of the combination of V940 and pembrolizumab compared to pembrolizumab alone.”
Poster: A retrospective look at treatment patterns and outcomes in patients with advanced endometrial cancer
Monday, June 3, 9:00AM
This retrospective study, led by Bhavana Pothuri, MD, director of gynecologic oncology research at Perlmutter Cancer Center and a professor in the Department of Obstetrics and Gynecology, assesses testing for treatment options, treatment patterns, and outcomes among patients with advanced endometrial cancer. In the past decade, newer therapies have been introduced for advanced endometrial cancer. Molecular profiling of mismatch repair/microsatellite instability (MMR/MSI) status has become an important testing tool to determine treatment, but real-world data on the prevalence of its use is limited.
Researchers looked at 1,441 deidentified patients with advanced endometrial cancer who started therapy between January 2018 and June 2023, analyzing patient characteristics, treatment patterns, and testing patterns.
While MMR/MSI testing was common, less than 50 percent of patients were receiving new therapies, and further study with implementation science may aid in increased adoption.
“Advanced endometrial cancer is the fourth most common cancer affecting women in the United States, and it is the only gynecologic malignancy with increasing incidence—and increasing mortality that is soon expected to surpass that of ovarian cancer,” said Dr. Pothuri. “Despite increasing trends, there may be outstanding barriers to the adoption of new therapies. We need further studies to assess these changes in outcomes over a longer time frame, along with continued education to increase awareness and access to newer FDA-approved treatments.”
Poster: The safety and efficacy of a noninvasive combination treatment for patients with recurrent glioblastoma
Saturday, June 1, 9:00AM
Dimitris G. Placantonakis, MD, PhD, an associate professor in the Department of Neurosurgery, is presenting an ongoing, multicenter phase 1/2 study that explores if sonodynamic therapy is safe and can help patients with recurrent or progressive glioblastoma live longer.
Recurrent glioblastoma is a lethal brain tumor that has an extremely poor prognosis and no effective therapies. Sonodynamic therapy is a noninvasive combination treatment that uses a drug, aminolevulinic acid HCL (SONALA-001), and a device, the Exablate 4000 Type 2.0, to deliver focused ultrasound to target glioblastoma cells. This has been shown in previous studies to lead to tumor cell death and improved survival in animal models.
People enrolled in this trial are receiving different dosage levels in order to determine the maximum tolerable dose for further study. The phase 2 portion will further characterize safety, along with evaluation of the efficacy of this treatment, with other key endpoints, including overall survival and recurrence rate.
“We are very excited about this study because, as a new therapy, it offers hope for people with this disease,” said Dr. Placantonakis. “This is also exciting because it offers a noninvasive treatment approach that pulses ultrasound waves from a device that is outside the head, so there is no need to surgically remove the tumor, and it eliminates the risk of side effects that are inherent in conventional brain surgery.”
Media Inquiries
Marlene Naanes
Phone: 646-754-5016
Marlene.Naanes@NYULangone.org