Dr. Frank Cecchin, director of pediatric and congenital electrophysiology at NYU Langone, with nurse practitioner Sharda McGuire and a young patient.
Photo: Beatrice DeGea
A few months ago, Jake Baxter decided to get rid of the device that had protected him for a decade from the cardiac disorder that killed his sister. Jake was born with a genetic mutation that could send his heart into a rapid arrhythmia—ending in cardiac arrest—at any time. As a teenager, he was surgically fitted with an implantable cardioverter-defibrillator (ICD), designed to detect dangerously irregular heartbeats and deliver a shock to set the rhythm back on course. However, he’d never actually experienced a cardiac event, and the business card–size gadget had never been activated. Now he was 24, and he wanted it out of his chest.
The reason was purely practical: He’d set his sights on a career as an electrical lineman, and after passing a series of grueling exams, he’d been accepted into the union. Then he learned that anyone with an ICD was disqualified from working with power lines, because electrical interference could cause the device to malfunction. For a worker 50 feet up a utility pole, a jolt from a misfiring defibrillator could have disastrous consequences.
Frustrated, Jake went to see Frank Cecchin, MD, director of pediatric and congenital electrophysiology at NYU Langone Medical Center, who had overseen his ICD’s maintenance since implanting it in 2005. From previous conversations with the doctor, the young man knew that for patients with his condition, the risk of cardiac arrest may decline after age 20. “I don’t really need this thing anymore,” he pleaded. “Can’t we just chuck it?”
“Maybe we can,” Dr. Cecchin (pronounced “check-een”) told him. “But before we move ahead, let me do a little more research.”
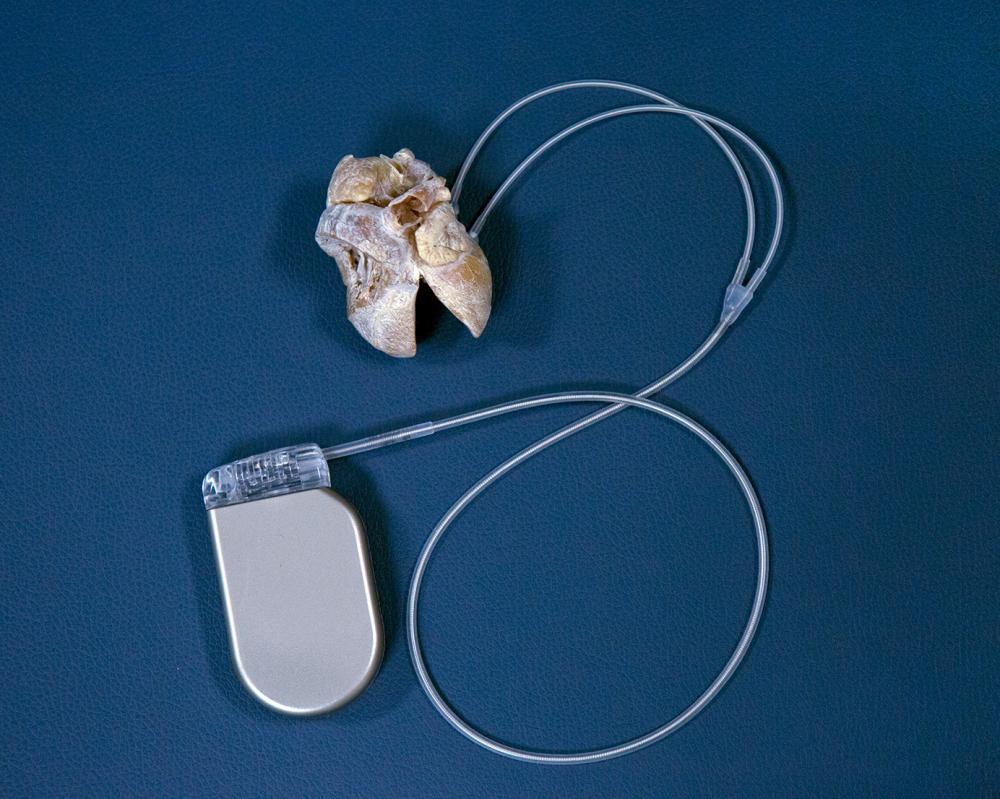
For children at risk of fatal cardiac arrhythmias, an ICD can greatly improve the odds of long-term survival. First introduced in 1980, the devices were used almost exclusively in adults until the 1990s, when advances in electronics and computing allowed them to be made small enough to fit inside a child’s chest. The basic version consists of a titanium box, or generator (containing computer circuitry, a capacitor, and a battery), and a wire known as the lead. In most patients, the generator is implanted in the left side of the chest, under the skin or muscle, and the lead is threaded through a vein into the chambers on the right side of the heart. Sensors relay heart rhythms to the ICD’s microprocessors. If potentially life-threatening tachycardia or fibrillation persists for too long, the generator interrupts these very chaotic, fast rhythms by sending a surge of energy to an electrode in the right ventricle.
ICDs are used for two broad purposes: primary prevention, which means warding off sudden cardiac arrest in high-risk patients, and secondary prevention, which means avoiding a recurrence in those who’ve already endured such an episode. Newer ICDs can also double as pacemakers, delivering pulses of low-voltage electricity to keep the heart from beating too slowly. The device can be implanted in infants as soon as a few weeks after birth. In these patients, the generator is implanted in the abdomen, where there’s enough space to accommodate it, and the leads are routed to the outside of the heart. In patients like Jake, who may experience sporadic arrhythmias, an ICD can function like a sprinkler system, kicking in if a biochemical glitch ignites a cardiac inferno.
Yet ICDs are difficult to live with. Batteries run out every five years or so, requiring surgery to replace the device. Leads can wear out or fracture, sometimes triggering a painful and terrifying storm of shocks. Even when an ICD does what it’s designed to do, zapping a runaway heartbeat into submission, the sensation is scary—a kick in the chest that can leave even a strong man reeling. For children, there are additional challenges. Their higher activity levels and growing bodies put more stress on the hardware, necessitating more frequent equipment changes and posing a greater potential for complications. If a lead creates scarring in a vein, for example, it must be rerouted. After several such operations, a child can run out of viable pathways.
The most daunting downside for pediatric ICD patients may be psychological. “You’re completely dependent on that device functioning properly,” observes Dr. Cecchin. “That knowledge affects all age groups, but it can have a huge impact on kids.” Several studies show that children with ICDs have far higher rates of anxiety than healthy kids. According to a paper he coauthored in the journal Pediatrics, incidence rises with children’s age at implantation and the severity of the disorder under treatment. “It’s enormously stressful for the parents as well,” notes nurse practitioner Sharda McGuire, who often recommends counseling for both patients and family members.
The devices and the doctors who prescribe them can sometimes reinforce recipients’ sense of insecurity. More than 20 percent of pediatric ICD patients experience inappropriate shocks, whether due to a broken lead or to misidentification of a harmless arrhythmia. Many cardiologists add to young patients’ angst by forbidding activities that could hypothetically damage the implant, such as sports in which collisions or falls are common. They may retain the ICD’s factory settings, which program it to fire the moment a ventricular tachycardia (an arrhythmia originating in the heart’s lower chambers) reaches 160 beats per minute. Better to suffer an unnecessary shock, goes the thinking, than to risk ventricular fibrillation, in which the rhythm becomes so rapid and disorganized that the heart stops pumping altogether.
“I tell children that this device is not there to stop you from doing anything," says Frank Cecchin, MD, director of pediatric and congenital electrophysiology at NYU Langone. “It’s there to enable you to do things safely.”
Over his 20 years as a pediatric cardiac electrophysiologist, Dr. Cecchin has developed a more nuanced approach to the problem of risk in his young patients—one informed by clinical studies showing that safety and flexibility are not always incompatible. In programming ICDs, he says, “we’ve learned not to be too aggressive. In children, a lot of arrhythmias are short-lived and resolve themselves. We wait for the maximum time possible to deliver a shock.” Thanks to that strategy and improved computer algorithms, he reports, none of his patients has experienced an unnecessary shock in at least two years. Nor have their devices failed to fire when truly needed.
Rather than issue blanket bans on strenuous exertion, Dr. Cecchin carefully considers each patient’s condition, discusses the possible dangers, and leaves the decision up to the individual. “If I say, ‘You can’t do this,’ they get angry, and they usually do it anyway,” he explains. “But if I give them an open door, they usually make the right choice.”
In fact, he points out, recent studies show that even rough sports seldom cause damage to ICDs. Except in rare cases, he encourages patients to be as active as they can. “I tell children that this device is not there to stop you from doing anything. It’s there to enable you to do things safely. If something happens, we’ll deal with it. The bottom line is that you have to enjoy life.”
If, in some cases, that might mean removing an ICD, he’s willing to consider it.
Jake Baxter is fair-haired and athletic, and the name of his late sister is tattooed over his heart. Rebecca was 13 in July 2000, the second of three children born to a pair of science teachers. She’d just finished eighth grade at Mansfield Middle School in Storrs, Connecticut, where she’d played basketball, softball, and soccer. She was a strong swimmer, too. So when she drowned in the shallow end of a public pool, her family’s grief was accompanied by bafflement. The autopsy revealed that the cause of death was sudden cardiac arrest. “It was a mystery,” recalls Jake, who was nine at the time. “We were all just blindsided.”
There was one clue, however: Rebecca’s father, Ed, had lost two brothers to drowning, both before they turned 18. A physician friend, suspecting that an inherited electrophysiological disorder might be the culprit, referred the Baxters to Dr. Cecchin, who was then practicing at Boston Children’s Hospital and whose own family had been touched tragically by cardiac disease.
The son of Italian immigrants, Frank Cecchin grew up in the Bronx and Long Island, where his father worked as a tile setter. His parents never made it past sixth grade, and they were fiercely proud of their high-achieving son. But his dad died of a heart attack during Frank’s first year of medical school. That event influenced his choice of specialties and helped shape his attitude toward his patients. “Dr. Cecchin is very warm and welcoming,” says Jake. “He makes you feel like he has all the time in the world for you.” Adds Jake’s mother, Judith: “He’s incredibly persistent. He wouldn’t give up until he figured out how to help us.”
Over the next two years, Jake and his sister Sarabeth, then 21, traveled to Boston for countless stress tests meant to spur a telltale arrhythmia. None of them yielded an abnormal graph line. Dr. Cecchin even immersed the siblings’ faces in ice water (which Jake recalls enjoying), but the electrocardiogram remained unperturbed. Then, at a professional conference, he met a Mayo Clinic scientist who was researching rare mutations in genes governing cardiac cells. Dr. Cecchin sent him a tissue sample from Rebecca’s autopsy, and blood samples from Jake, Sarabeth, and their father. In June 2004, the results came back. All the specimens showed a mutation that causes a rhythm disorder called catecholaminergic polymorphic ventricular tachycardia (CPVT).
CPVT stems from a defect in the body’s calcium channels, proteins that control the passage of certain electrochemical signals—carried by calcium ions—between cells. (Other rhythm disorders, such as long QT or short QT syndrome, involve different types of ion channels.) It’s believed to affect about 1 in 10,000 people, and to be responsible for 15 percent of unexplained sudden cardiac deaths in youngsters. Warning signs may include dizziness or fainting in response to intense exercise or emotional stress. In some cases, however, the first symptom is cardiac arrest.
To prevent that from happening, Dr. Cecchin offered two choices: an ICD or a lifetime of exercise restriction and beta-blockers, which prevent tachycardia by blunting the heart rate. Jake’s father opted for the medication. Jake—an avid mountain biker and snowboarder—chose the device. So did Sarabeth, and so did several of their aunts and cousins after they tested positive for CPVT.
Jake was 13 when he received the implant. Although he agreed to give up swimming, he soon returned to his other rugged pursuits. At 15, he joined a downhill mountain-bike team and began racing every weekend. By the time he finished high school, he’d competed on single tracks from Canada to California. He went on to junior college, earning a certification in sustainable energy. Then, he began studying to become an electrical lineman.
Meanwhile, in 2013, Dr. Cecchin moved from Boston to NYU Langone, lured there by Achiau Ludomirsky, MD, the Andrall E. Pearson Professor of Pediatric Cardiology and director of the Division of Pediatric Cardiology, who’d been his fellowship adviser at Texas Children’s Hospital. “I’d been trying to recruit him for ages,” says Dr. Ludomirsky. “I consider him one of the best pediatric electrophysiologists in the country, maybe the world.”
After Jake visited his office last winter, Dr. Cecchin set to work trying to determine whether it was safe to remove the young man’s ICD. Although the odds of sudden death from CPVT fall sharply in adulthood, he knew that different variants of the disorder could follow different courses. He began combing through the literature in search of other patients with the precise mutation shared by Jake and his relatives.
No one else turned up with that particular glitch, but there were a few cases of mutations on DNA base pairs just a rung or two away on the ryanodine receptor gene. Some of those patients, Dr. Cecchin discovered, had died of cardiac arrest in their 30s.
When Jake got the news, he came to a new decision: the implant would stay in; working on power lines was out. He would keep his current job, driving trucks for the department of public works. But he didn’t surrender to the status quo. Instead, he turned his energy to another project, a small industrial-prototype business that he’d founded with a friend. The startup aims to specialize in developing prostheses for bike riders with disabilities.
“My defibrillator has never held me back from what I love to do,” Jake says, “and it’s good to know that someday, it just might save my life.”