Controlling high blood pressure is key to avoiding dementia—and it’s never too early to start.
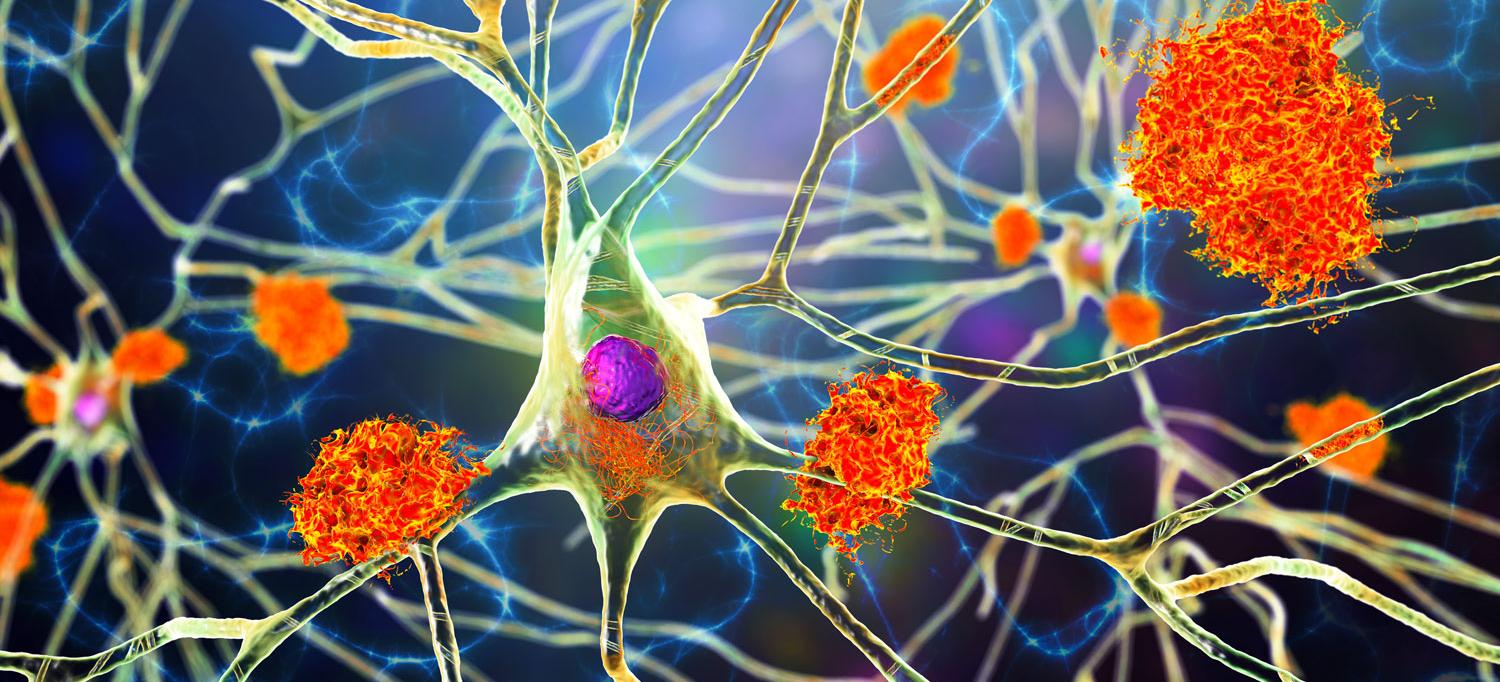
An illustration of amyloid plaques—a characteristic feature of Alzheimer's disease. Controlling high blood pressure can help prevent Alzheimer’s and all other kinds of dementia.
Credit: GETTY/KATERYNA KON/SCIENCE PHOTO LIBRARY
To mark Alzheimer’s and Brain Awareness Month, we spoke to Josef Coresh, MD, PhD, director of NYU Langone’s Optimal Aging Institute, about the connection between high blood pressure and dementia, including Alzheimer’s disease. An internationally known expert in aging and the effects of vascular disease on the brain, Dr. Coresh conducts research aimed at improving the health of older people.
Here are his takeaways.
High Blood Pressure in Midlife Is a Powerful Predictor of Alzheimer’s Disease in Later Life.
Many people are aware that high blood pressure, or hypertension, can lead to heart disease and stroke. You may not know that it’s also an early warning sign of dementia.
“Research shows that people with high blood pressure in their early 40s to early 60s are significantly more likely to develop dementia, including Alzheimer’s disease,” says Dr. Coresh.
Why? High blood pressure damages blood vessels and causes blockages that reduce blood flow to the brain. It reduces the blood’s ability to clear harmful waste products and breaks down connectivity between areas of the brain.
These harmful effects develop and take place over years and even decades, well before symptoms of dementia begin to appear.
But what constitutes high blood pressure? Since 2017, the American College of Cardiology has divided high blood pressure into two stages. Stage 1 occurs when the top number, or the systolic pressure, is 130 to 139 and the bottom number, or the diastolic number, is 80 to 89. Stage 2 is when the top number is 140 to 180 and the bottom number is 90 to 120. People with stage 2 high blood pressure may require more-aggressive treatments.
It’s Never Too Early to Control High Blood Pressure.
“We know that controlling blood pressure in your 60s can decrease your chances of developing dementia by 15 percent,” says Dr. Coresh. “It might decrease by double that if you started a decade or two earlier.” The bottom line? You’re never too young to pay attention to your blood pressure.
Aim for 120/80.
What is a healthy blood pressure reading? “Ideally people should get their blood pressure below 120/80,” says Dr. Coresh. That said, benefits come from any reduction. “In the biggest trials,” he says, “people aimed for 120 and got closer to 130. That’s probably still beneficial.”
Measure Your Blood Pressure at Home.
Dr. Coresh is a proponent of home blood pressure monitors, and not just because some people experience elevated blood pressure at the doctor’s office, a phenomenon known as white coat syndrome.
For the most accurate reading, you should first go to the bathroom to try to urinate and then rest quietly for five minutes. While taking the reading, you should sit straight, with both feet flat on the floor, and place the blood pressure cuff on bare skin. Finally, take two readings, one minute apart. “Things are often rushed at the doctor’s office,” says Dr. Coresh, “and so they’re often not able to take all of those steps.”
Blood pressure monitors have become fairly inexpensive in recent years. And many flexible spending accounts now reimburse the purchase price. “A lot of the monitors are now Bluetooth equipped, which allow you to track your readings over time and share them with your doctor,” says Dr. Coresh. Failing that, record your readings in a notebook or on your phone.
Don’t Defer Medication.
In the past, doctors sometimes prescribed blood pressure–lowering medication only after weight loss, improvements in diet, and exercise were unsuccessful. “The preferable way,” says Dr. Coresh, “is to try dietary changes and medication simultaneously. If you want to get to 120 systolic (the high number), you’re going to need both.”
See Your Doctor
You don’t have to navigate high blood pressure alone. NYU Langone cardiologists specialize in diagnosing the condition and choosing the optimal tools and treatments for your needs and lifestyle. Take the first step and schedule with a doctor near you.