The combination of two new drugs that harness the body’s immune system is safe and effective, destroying most cancer cells in 64 percent of patients with recurrent Hodgkin lymphoma, according to the results of an early-phase study led by NYU Langone Medical Center.
Presented December 5 at the annual meeting of the American Society of Hematology in San Diego, the study in 19 patients found that the combination of brentuximab vedotin, marketed as Adcetris®, and nivolumab, known as Opdivo®, decreased tumor size or spread (achieved remission) to some degree in all patients after 3 months of treatment.
Researchers say the dual therapy was “generally well tolerated,” with “manageable” side effects, such as itchiness and rash, and that only two patients who experienced inflammation in the lungs were withdrawn from treatment.
The multicenter clinical trial, led by a researcher at the Perlmutter Cancer Center at NYU Langone, was conducted in patients for whom initial chemotherapy or stem cell transplantation had failed to stop cancer cell growth. The research team says its latest results extend work presented at the same meeting in 2015, which found that a similar combination, with brentuximab vedotin and ipilimumab, marketed as Yervoy®, also was safe and highly active against lymphoma.
“Although our study offers reason for optimism, the results of larger, longer-term studies already underway are needed before combination immunotherapy could become the new standard of care for people whose Hodgkin lymphoma returns after initial treatment,” says study lead investigator and hematologist–oncologist Catherine S. Diefenbach, MD. The disease, she notes, affects mostly those under age 40, with 1 in 10 experiencing relapse, leading to some 1,300 deaths per year. Most cases of Hodgkin lymphoma are considered curable if diagnosed and treated early.
“If further testing proves successful, such dual therapies could potentially become an alternative curative regimen for relapsed Hodgkin lymphoma,” says Diefenbach, an assistant professor at NYU Langone and clinical director of lymphoma program services at the Perlmutter Cancer Center.
Diefenbach says the team’s experiments were inspired by her laboratory’s research in 2012, which had found that in patients with Hodgkin lymphoma, the workhorses of the immune system, or circulating T cells, showed signs of immune dysfunction that could make them less likely to be activated.
This led her and her colleagues to test whether drugs that spur the immune system to attack cancer cells, such as “checkpoint inhibitors” like nivolumab and ipilimumab, would work well with targeted chemotherapy with brentuximab vedotin, a drug known as an antibody–drug conjugate.
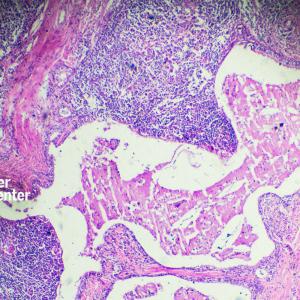
Like a Trojan horse, researchers say, brentuximab vedotin homes in on CD30, a protein on the surface of some Hodgkin lymphoma cells, and then delivers an attached dose of chemotherapy to destroy the cell. Nivolumab turns off an inhibitory switch, or “checkpoint,” called PD1 on T cell surfaces, which is known to prevent the immune system from identifying and attacking tumor cells. Ipilimumab targets a different checkpoint, called CTLA4.
Moving forward, Diefenbach says she hopes to apply the concepts from this treatment strategy to other types of non-Hodgkin lymphoma.
Funding support for the study, known formally as the ECOG-ACRIN Cancer Research Group, was provided by National Cancer Institute grants R01 CA180820, R01 CA180794, R01 CA180864, R01 CA180795, R01 CA180802, R01 CA180816, R01 180799, and R01 CA180790.
Besides Diefenbach, other study investigators involved in this research are Fangxin Hong, MD, at the Dana Farber Cancer Institute in Boston; Kevin David, MD, at Rutgers Cancer Institute of New Jersey; Jonathon Cohen, MD, at Emory University in Atlanta; Michael Robertson, MD, at Indiana University Hospital in Indianapolis; Ranjana Advani, MD, at Stanford University in California; Neil Palmisiano, MD, at Penn State Milton S. Hershey Cancer Center; Richard Ambinder, MD, at Johns Hopkins Kimmel Cancer Center in Baltimore; Brad Kahl, MD, at Washington University in St. Louis, Mo.; and Stephen Ansell, MD, at the Mayo Clinic in Rochester, Minn.
Media Inquiries
David March
Phone: 212-404-3528
david.march@nyumc.org