Photo: jxfzsy/Getty
A half century ago, people with Hodgkin lymphoma, a blood cancer that affects primarily young adults, had few options for treating the disease. Chemotherapy was available, but the side effects, which included infertility and the development of secondary lymphomas and other cancers, did not lead to cures. Today, Hodgkin lymphoma has become one of the most curable forms of cancer.
Although up to 80 percent of people with the common form of Hodgkin lymphoma control the disease over the long term with initial treatment, approximately 1,200 primarily young people in the United States die annually because of disease that relapses or does not respond to treatment.
Research Aims to Expand Treatment for Relapsed Hodgkin Lymphoma
Catherine S. Diefenbach, MD, director of the Clinical Lymphoma Program at NYU Langone Health’s Perlmutter Cancer Center, currently leads a national phase 1/2 randomized clinical trial for people with relapsed Hodgkin lymphoma.
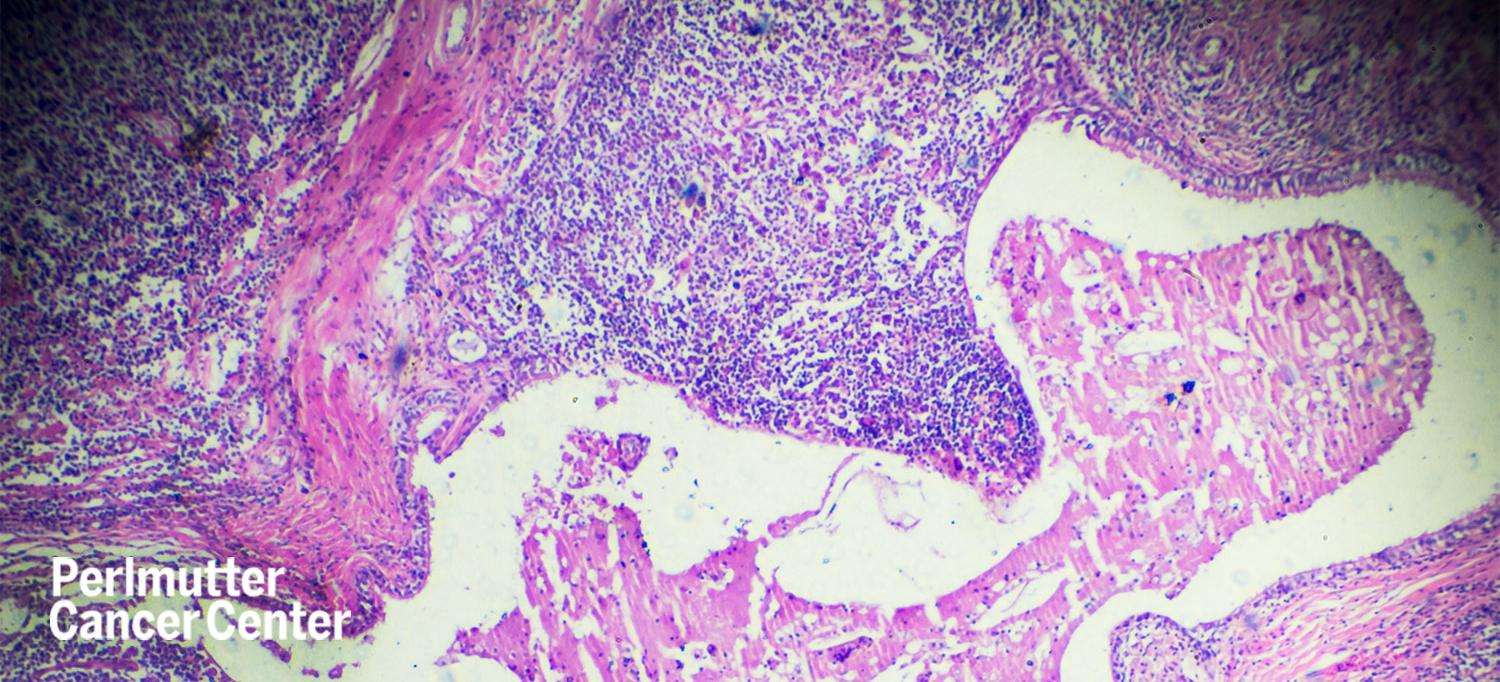
Hodgkin lymphoma is an unusual tumor with a paucity of tumor cells in a microenvironment that is full of dysfunctional immune cells. The treatment Dr. Diefenbach and her colleagues are testing in the clinical trial uses brentuximab vedotin. An antibody–drug conjugate, brentuximab vedotin is a highly specific medicine that comprises a small molecule cancer drug attached to a monoclonal antibody. Brentuximab vedotin was approved by the U.S. Food and Drug Administration in 2018 as the first new drug to treat Hodgkin lymphoma in more than 20 years.
Preliminary data generated by Dr. Diefenbach and her colleagues through early preclinical work showed that circulating T cells in people with Hodgkin lymphoma were exhausted, or lost their ability to fight cancer, compared with cells of healthy people. Using this preliminary data, Dr. Diefenbach was able to initially obtain approval of a single-arm phase 1 clinical trial through the National Cancer Institute (NCI)–sponsored cooperative group ECOG-ACRIN—formed by the merger of the Eastern Cooperative Oncology Group and the American College of Radiology Imaging Network—combining brentuximab vedotin and an immunotherapy drug called ipilimumab.
“My colleagues and I pioneered the concept of directing targeted chemotherapies to the few tumor cells that are present while activating immune cells in the tumor microenvironment that were protecting and promoting tumor cell growth,” says Dr. Diefenbach, an associate professor in the Department of Medicine and director of hematology translational research at Perlmutter Cancer Center. “This therapy proved to be safe and highly active in patients with relapsed Hodgkin lymphoma.”
The success of the initial trial led Dr. Diefenbach to expand the study to include the additional immunotherapy nivolumab, and to combine ipilimumab and nivolumab with brentuximab vedotin. The trial was further developed into a randomized phase 2 study comparing the combination of brentuximab vedotin and nivolumab with the triplet of brentuximab vedotin, ipilimumab, and nivolumab to determine whether the triplet regimen is more active than the brentuximab vedotin with nivolumab regimen, with manageable toxicity.
“We should have data from this trial within a year or so, but the results so far have been very exciting,” Dr. Diefenbach says. The phase 1 clinical trial data was published earlier this year in The Lancet Hematology.
A phase 3 study is in the early planning stages that aims to evaluate whether one of the regimens should become a standard second-line therapy as a bridge to stem cell transplant, or whether some second-line patients could use the most effective regimen of this study as a therapy in place of stem cell transplant, Dr. Diefenbach says.
National Cancer Act Spurs Research, Improved Treatment
Funding provided by the NCI makes research by Dr. Diefenbach and other cancer researchers at Perlmutter Cancer Center possible. This year, the NCI celebrates the 50th anniversary of the National Cancer Act, which was signed into law by President Richard Nixon in December 1971.
From 1991 to 2018, the cancer death rate decreased 31 percent, according to statistics compiled by the American Cancer Society, including a record 1-year drop of 2.4 percent from 2017 to 2018. Much of this progress can be attributed to the National Cancer Act.
Among its many accomplishments, the act led to the creation of the first NCI-designated cancer centers, including Perlmutter Cancer Center, 1 of 51 NCI-designated Comprehensive Cancer Centers in the United States.
The National Cancer Act also led to the expansion of NCI’s cancer clinical trials networks, which enable researchers to conduct critically important patient-oriented research that has resulted in the development of treatments for people with cancer that can prolong life and, for some cancers, enable people to live cancer-free.
Clinical Trials Offer New Options
At Perlmutter Cancer Center, clinical trials offer new options for people with advanced cancer, including new drugs and new combination therapies. And by participating in clinical trials, patients get first access to potentially lifesaving treatments while advancing knowledge that will help future generations.
The combination of brentuximab vedotin and immunotherapy drugs that Dr. Diefenbach pioneered and is testing in clinical trials demonstrates that some patients have durable responses, making these regimens a highly active therapy for relapsed Hodgkin lymphoma, which can allow more patients to proceed to stem cell transplant and allow patients who have relapsed after stem cell transplant to have durable disease control.
“This novel treatment appears to result in excellent outcomes for patients who subsequently go to stem cell transplant, and it may allow a subset of patients to be cured without a stem cell transplant,” Dr. Diefenbach says. “How to position this therapy, and who should be treated with it, are exciting research questions for the future. Our goal for the future is to tailor lymphoma treatments to cure more patients, with therapies that are more clearly tailored to disease biology and are more effective with less toxicity.”