Photo: Hailshadow/Getty
Patients hospitalized for COVID-19 had higher levels over the short term of blood proteins known to rise with neurological damage than non–COVID-19 patients diagnosed with Alzheimer’s disease, a new study finds.
Importantly, the current report, published online January 13 in Alzheimer’s & Dementia®: The Journal of the Alzheimer’s Association, was conducted over two months early in the COVID-19 pandemic (March to May 2020). Any determination of whether patients with COVID-19 are at increased risk for future Alzheimer’s disease, or instead recover over time, must await the outcomes of long-term studies.
Led by researchers at NYU Grossman School of Medicine, the new study found higher levels of seven markers of brain damage (neurodegeneration) in patients with COVID-19 with neurological symptoms than those without them, and much higher levels in patients that died in the hospital than in those discharged and sent home.
A second analysis found that a subset of the damage markers in patients hospitalized with COVID-19, over the short term, were significantly higher than in patients diagnosed with Alzheimer’s disease, and in one case more than twice as high.
“Our findings suggest that patients hospitalized for COVID-19, and especially in those experiencing neurological symptoms during their acute infection, may have levels of brain injury markers that are as high as, or higher than, those seen in people who have Alzheimer’s disease,” says lead author Jennifer A. Frontera, MD, professor in the Department of Neurology at NYU Grossman School of Medicine.
Study Structure and Details
The current study identified 251 people that, although 71 years on age on average, had no record or symptoms of cognitive decline or dementia before being hospitalized for COVID-19. These patients were then divided into groups with and without neurological symptoms during their acute COVID-19 infection, when patients either recovered and were discharged, or died.
The research team also, where possible, compared marker levels in the COVID-19 group to patients in the Clinical Core cohort of NYU Langone’s Alzheimer’s Disease Research Center, an ongoing, long-term study at NYU Langone Health. None of these 161 control patients (54 cognitively normal, 54 with mild cognitive impairment, and 53 diagnosed with Alzheimer’s disease) had COVID-19. Brain injury was measured using single-molecule array (SIMOA) technology, which can track the minute blood levels of neurodegeneration markers in picograms (one trillionth of a gram) per milliliter of blood (pg/ml), where older technologies could not.
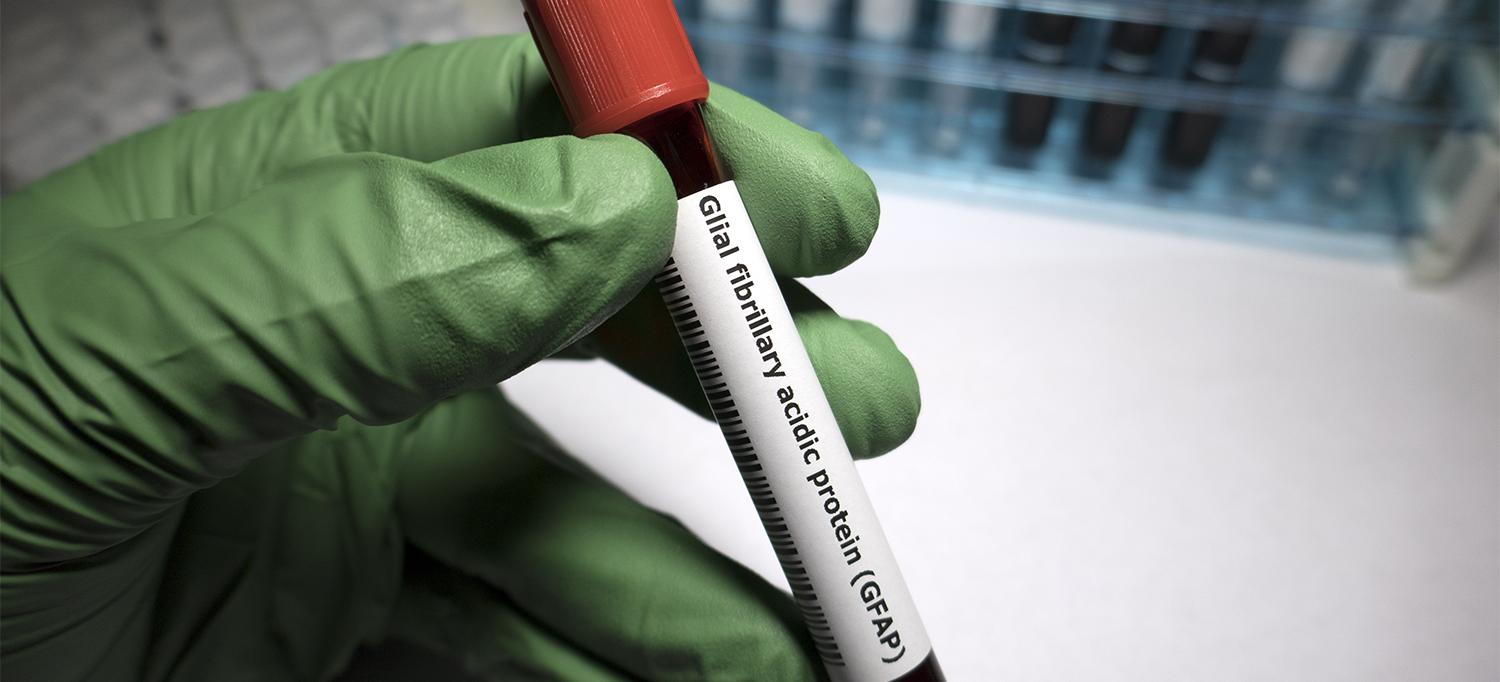
Three of the study markers—ubiquitin carboxy-terminal hydrolase L1 (UCHL1), total tau, and phosphorylated-tau-181 (ptau181)—are known measures of the death or disabling of neurons, the cells that enable nerve pathways to carry messages. Levels of neurofilament light chain increase with damage to axons, which are extensions of neurons. Glial fibrillary acidic protein (GFAP) is a measure of damage to glial cells, which support neurons. Amyloid beta 40 and 42 are proteins known to build up in people who have Alzheimer’s disease. Past study results argue that total tau and ptau181 are also specific measures of Alzheimer’s disease, but their role in the disease remains a matter of debate.
Blood markers in the COVID-19 patient group were measured in blood serum (the liquid part of blood that has been made to clot), while those in the Alzheimer’s disease study were measured in plasma (the liquid blood fraction that remains when clotting is prevented). For technical reasons, the difference meant that neurofilament light chain, GFAP, and UCHL1 levels could be compared between the COVID-19 group and patients in the Alzheimer’s disease study, but total tau, ptau181, amyloid beta 40, and amyloid beta 42 could only be compared within the COVID-19 patient group (neuro symptoms or not; death or discharge).
Further, the main measure of neurological damage in patients with COVID-19 was toxic metabolic encephalopathy, or TME, with symptoms that range from confusion to coma, and caused during severe infections by toxins generated as the immune system overreacts (sepsis), kidneys fail (uremia), and oxygen delivery is compromised (hypoxia). Specifically, the average percentage increase in levels of the 7 markers for hospitalized patients with TME compared to those without neurological symptoms was 60.5 percent. For the same markers within the COVID-19 group, average percentage increase when comparing those successfully discharged home from the hospital to those who died in the hospital was 124 percent.
A secondary set of findings came from comparing neurofilament light chain, GFAP, and UCHL1 levels in the serum of people with COVID-19 against levels of the same markers in the plasma of non–COVID-19 Alzheimer’s disease patients. Neurofilament light chain was, over the short-term, 179 percent higher (73.2 versus 26.2 pg/ml) in patients with COVID-19 than those with Alzheimer’s disease. GFAP was 65 percent higher (443.5 versus 275.1 pg/ml) in patients with COVID-19 patients than those with Alzheimer’s disease, while UCHL1 was 13 percent higher (43 versus 38.1 pg/ml).
“Traumatic brain injury, which is also associated with increases in these biomarkers, does not mean that a patient will develop Alzheimer’s disease or related dementias later on, but does increase the risk of it,” says senior author Thomas M. Wisniewski, MD, the Gerald J. and Dorothy R. Friedman Professor in the Department of Neurology and director of the Center for Cognitive Neurology at NYU Langone. “Whether that kind of relationship exists in those who survive severe COVID-19 is a question we urgently need to answer with ongoing monitoring of these patients.”
Along with Dr. Frontera and Dr. Wisniewski, NYU Langone Health authors were first author Allal Boutajangout, PhD; Arjun V. Masurkar, MD, PhD; Yulin Ge, MD; Alok Vedvyas; Ludovic Debure; Andre L. Moreira, MD; Ariane Lewis, MD; Joshua Huang; Sujata P. Thawani, MD, MPH; Laura J. Balcer, MD; and Steven L. Galetta, MD. Also an author was Rebecca Betensky at NYU School of Global Public Health. This study was funded by a grant from the National Institute on Aging COVID-19 administrative supplement 3P30AG066512-01.
Media Inquiries
Greg Williams
Phone: 212-404-3500
gregory.williams@nyulangone.org