Facial plastic and reconstructive surgeons at NYU Langone, including Dr. Judy W. Lee, are experts in a new surgical approach that sets the standard of care for facial paralysis.
Photo: Karsten Moran
An advanced facial reanimation approach pioneered by surgeons at NYU Langone’s Facial Paralysis and Reanimation Center is providing patients who have facial paralysis with greater spontaneous movement and functional improvement following surgery. The nuanced, multi-graft technique is showing positive results in cases of complete and partial facial paralysis. The surgery closely mirrors facial nerve anatomy, enabling nerve specialization that gives patients different levels of control over facial segments—and better functional outcomes.
Circumventing Synkinesis, Nerve by Nerve
For patients with total facial paralysis, the new technique takes a more sophisticated approach to facial nerve grafting to circumvent the problem of synkinesis—often experienced by patients following single-graft reanimation surgery. In that more commonly used approach, either the main trunk or a single division of the facial nerve is attached to a single nerve such as the hypoglossal or accessory, resulting in mass movement of the facial nerve. For patients, this means the loss of control of independent motions, such as smiling accompanied by involuntary eye movements.
“The traditional reanimation surgery oversimplifies the complex anatomy of the facial nerve, which breaks into three divisions and five segments for five areas of facial function, all with very specific jobs to innervate the face,” explains Adam S. Jacobson, MD, associate professor in the Department of Otolaryngology—Head and Neck Surgery, chief of the Division of Head and Neck Surgery, and co-director of the Head and Neck Center. “So when you connect the main nerve trunk of the facial nerve to another large nerve, how do the axons growing through the nerve know how to go to very specific facial segments to give independent control? They don’t—and that’s what causes synkinesis, a suboptimal outcome for patients’ quality of life. We wanted to improve upon this technique for our patients.”
Segmenting the Face to Restore Specific Functions
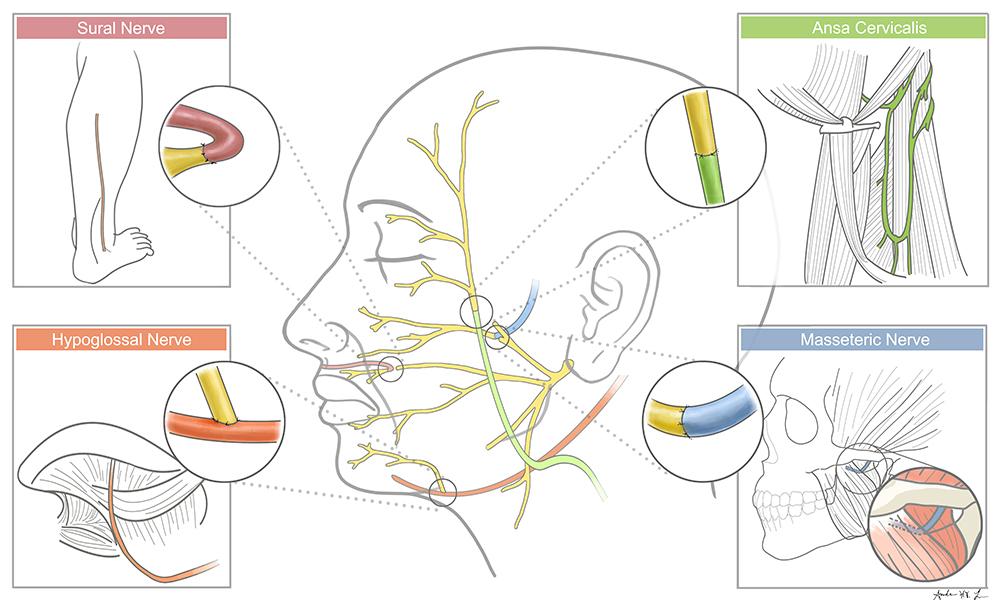
In the new approach, the distal ends of each division of the facial nerve are attached to different regional nerves. By segmenting the function of the facial nerve into regions and providing different sources of innervation, the surgeons give each division of the facial nerve independent control, approaching the pre-disease state. The masseter nerve is connected to the distal end of the midface division, the lower division of the facial nerve is connected to the hypoglossal nerve to animate the lower face, and the ansa cervicalis is connected to the upper division of the face to give tone to the eye muscles. In some cases, a cross-face nerve graft is used to innervate the affected midface with input from the intact contralateral midface division. The more nuanced procedure typically involves three to four nerve grafts from different parts of the body, transposed and connected across the face to innervate each area independently.
“This more dynamic reconstruction technique takes longer in the operating room because we are harvesting and rotating or transferring multiple nerves and attaching them to more specific areas of the face,” notes Judy W. Lee, MD, assistant professor of otolaryngology—head and neck surgery and director of both the Facial Paralysis and Reanimation Center and Division of Facial Plastic and Reconstructive Surgery. “We’re giving multiple inputs to the damaged nerves, so over time they start sequentially taking over and giving different levels of control to the segments of the face.”
The procedure, found to be well tolerated without additional complications over the traditional approach, offers the benefit of stepwise improvement, with each patient experiencing unique functional recovery between 3 and 12 months postoperatively as the new nerve inputs reanimate the previous areas of paralysis. “The masseter nerve is very powerful and grows wherever you connect it, so we’ve seen it begin to innervate the muscle there as early as three to six months postoperatively,” adds Dr. Lee.
With this new surgical option, patients with total facial paralysis can now receive treatment that not only restores movement, but also provides more natural facial function—an improvement in outcomes that enhances their quality of life and sets a new standard of care.
Promising Applications for Innovative Local Nerve Transfers
A variation on the new technique offers additional promise for patients recovering from Bell’s palsy, a process that can incur complications when nerve axons regenerate into the wrong locations, causing synkinesis. Selective neurectomy removes problematic axons, which, combined with local nerve transfer, can restore controlled facial movement.
Similarly, a multidisciplinary collaboration with neuro-otologists is helping to identify patients with acoustic neuromas likely to be left with permanent functional nerve loss following resection—whether due to deterioration in the nerve from the condition itself or necessary elimination of the nerve during surgery. “Those patients can then be scheduled for nerve transfer surgery to restore controlled facial function—an immediate solution rather than a wait-and-see approach or the traditional facial reanimation approach,” explains Dr. Jacobson. “The sooner a nerve transfer surgery is performed after the injury, the better the functional outcomes for these patients.”