Thanks to scarless surgery, Caitlin Zerra Rose has nothing to hide. She has also regained her full vocal power, with the help of therapy at NYU Langone’s Voice Center.
Credit: Brad Trent
Caitlin Zerra Rose first noticed a lump on the left side of her neck in the spring of 2021. She chalked up the slight swelling—along with her thinning hair and swings between deep fatigue and restless energy—to stress. A vocalist and actress in her late twenties, Rose works in theater, film, and commercials, and as a singing waitress at a Times Square restaurant, amounting to a fulfilling but demanding livelihood and lifestyle.
By April 2023, the mass had become more prominent, so Rose visited an urgent care clinic to have it examined. An ultrasound revealed an inch-long nodule on Rose’s thyroid, the butterfly-shaped gland that secretes hormones vital to regulating metabolic functions, including heart rate, body temperature, sleep, and brain activity. Blood tests showed excessive levels of these hormones, a condition known as hyperthyroidism. When she googled the disorder, Rose learned that treatment sometimes requires an operation. “As someone whose profession depends on my voice and my appearance,” she says, “the idea of having surgery on my throat terrified me.”
Rose found her way to NYU Langone Health endocrinologist Priya Jaisinghani, MD, an expert on thyroid disorders. After running further blood and imaging tests, Dr. Jaisinghani explained that they indicated Hashimoto’s thyroiditis, an autoimmune disease in which the immune system attacks the gland. This can trigger temporary hyperthyroidism, spurring symptoms such as anxiety and hyperactivity. Over time, though, the disease mainly leads to excessively low levels of thyroid hormones, or hypothyroidism, causing a variety of symptoms, including lethargy and depression. It can also induce hair loss. Rose’s host of vague ills finally came into focus: they had all resulted, she realized, from these hormonal fluctuations.
Rose’s biopsy came back negative. “We decided that keeping watch on the nodule and her hormone levels was the best approach for the time being,” Dr. Jaisinghani says. Hyperthyroidism in thyroiditis is transient, while hypothyroidism associated with Hashimoto’s can usually be managed with thyroid hormone replacement medication. Surgery is needed only if a nodule tests positive for cancer (as it does in 5 to 10 percent of cases) or its molecular genetic profile suggests a possible malignancy.
Once Rose’s thyroid hormone levels dropped, Dr. Jaisinghani prescribed thyroid hormone replacement therapy. Yet a bigger challenge arose in May 2024, when an ultrasound showed that the nodule had grown to nearly 1.5 inches long by 1 inch wide. A subsequent biopsy detected mutations, suggesting the lesion could be cancerous or precancerous. “That was news I’d been praying not to hear,” Rose says.
Based on these suspicious findings, Dr. Jaisinghani advised that a thyroidectomy, the surgical removal of all or part of the gland, was the safest course. The next step was deciding whether to opt for a traditional “open” thyroidectomy or a less invasive procedure. When Rose expressed her preference for the latter, Dr. Jaisinghani recommended that she consult Insoo Suh, MD, director of minimally invasive endocrine surgery and vice chair for surgical innovation in the Department of Surgery.
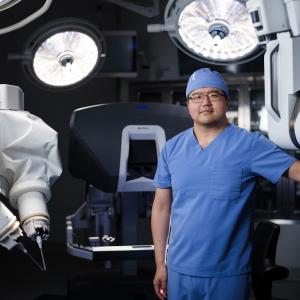
Dr. Suh leads a clinical and research program in “scarless” endoscopic thyroidectomy, an approach that avoids the long mark across the throat left by open surgery. “That visible scar is not a minor concern,” Dr. Suh notes. “My patients often say it’s not about vanity, but about seeing the scar every day in the mirror, reminding them of the disease and announcing their private health information to the world.” Although thyroid disorders are more common in women than men, he adds, such concerns transcend sex. Minimally invasive approaches are often favored by younger people and those in the performing arts, whose work can be adversely affected by a prominent scar.
Dr. Suh was among the earliest adopters in the United States of the first successful scarless technique, transoral endoscopic thyroidectomy vestibular approach (TOETVA). In 2018, he introduced his own innovative method, dubbed transoral and submental thyroidectomy (TOaST), an approach that improves on its predecessor in several important ways. In TOETVA, surgeons make three small incisions behind the patient’s lower lip and tunnel down to the thyroid though an endoscopic tube, guided by a tiny camera. The diseased tissue is removed through the middle incision. In TOaST, the central incision is made beneath the chin, reducing the potential for complications, including damage to facial nerves and muscles. Though TOaST does leave a small scar, the inconspicuous location makes it virtually unnoticeable. The position of the incision allows larger portions of tissue to be removed intact, yielding a specimen that is easier for pathologists to evaluate. TOaST also causes less postoperative pain and enables a quicker recovery.
Dr. Suh’s technique has been adopted worldwide, but NYU Langone is among only a handful of health systems in the country to offer it. At their first meeting, Rose was impressed with Dr. Suh’s description of the method as well as his kind and reassuring manner. “It felt as if the stars had aligned,” she says.
During the two-hour surgery in a Kimmel Pavilion operating room on September 30, 2024, Dr. Suh removed the left side of Rose’s thyroid. She awoke in a recovery bed and checked her vocal range with a quick glissando; it was unimpaired. “At that moment,” she recalls, “a huge weight slid off my shoulders.” To her further relief, the pathology report noted precancerous cells rather than a tumor.
Rose returned to her home in Harlem the next day. A week later, she was belting out show tunes at her restaurant job. By the spring of 2025, after vocal therapy at NYU Langone’s Voice Center with speech pathologist Taylor Darden, SLP, her pipes had regained their full presurgical power. She recently launched her own singing troupe, appearing at events across New York City.
Rose’s thyroid-related symptoms remain under control, thanks to medications and Dr. Jaisinghani’s continued vigilance. “I’m so grateful to everyone at NYU Langone,” she says. “They understand that part of my health is living the life I love. What brings me happiness has always been at the forefront of their minds.”