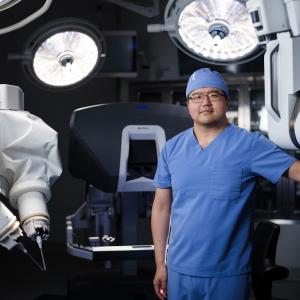
Emily Barkocy poses with members of her transplant team at NYU Langone’s Kimmel Pavilion the day of her initial discharge.
Imagine the worst flu symptoms ever, followed by crippling abdominal pain. Your doctor suspects your appendix has burst, so you head to the nearest emergency department. But tests reveal something entirely unexpected: your liver is shutting down.
Acute liver failure is a rare and sudden event affecting fewer than ten in a million people globally. Emily Barkocy of Rockaway, New Jersey, was one of those people. In just over the span of a week, the Morris Hills High School assistant principal went from handing out diplomas at commencement to being airlifted into Manhattan, where specialists at the NYU Langone Transplant Institute evaluated her for an emergency liver transplant.
Without a compatible organ and successful surgery, her story could have ended tragically. Today she describes the experience as a blessing. “It changed my life, but it also gave me new perspective,” says the 43-year-old, a vocal advocate for organ donation awareness.
Rising to the Top of the Liver Transplant List
On July 1, 2022, the community hospital where Barkocy initially sought care began calling transplant centers seeking to transfer its severely ill patient. She remembers the helicopter ride into the city but lost consciousness in the ambulance on the way to NYU Langone’s Kimmel Pavilion.
Waking up the following afternoon, Emily began to realize the gravity of her illness. Doctors explained that her liver was no longer functioning, and her kidneys were failing. “There was nothing filtering my blood,” she says. An interventional radiology team placed catheters in her neck to begin kidney dialysis.
As part of a pretransplant assessment, Barkocy fielded a battery of questions to gauge her cognitive function: What’s your address? What are your daughters’ names? “I felt myself starting to forget,” she admits. Adam Griesemer, MD, director of the living donor and pediatric transplant program, explains that when someone with acute liver injury becomes confused, “it’s a sign that the brain is starting to swell, and we don’t have much time to get the liver transplant done.”
Barkocy called her mother to break the news. While emotional, she never allowed herself to consider the possibility that she might not survive. “It was not an option for me to die,” she says, “because I had 4-year-old twins. They needed their mom.”
The team listed her for transplant on July 2. The next morning, her name appeared at the top of the list, reflecting the acute nature of her condition and the severity of her illness. “Falling critically ill so suddenly meant we had to treat her very quickly,” notes Karim J. Halazun, MD, surgical director of the adult liver transplant program. “Otherwise, she would have died.”
Implanting the Donor Organ
The Liver Transplant Program team assembled the morning of July 3. Dr. Halazun worked meticulously to separate Barkocy’s liver from all its attachments and gently place the donor liver in her body. The team watched and waited patiently as the new organ established proper blood flow. The entire procedure lasted 10 to 11 hours, including anesthesia time.
It was a textbook case, except for a kidney complication, which was related to her liver failure. When a person’s liver stops functioning, it stops making clotting factors and the blood thins out, explains Dr. Griesemer.
The next day, Dr. Halazun performed a second surgery to remove her right kidney due to uncontrolled bleeding.
“We’re So Glad You’re Alive”
The following days were a blank slate. Not until a nurse’s cheerful greeting roused Barkocy did she learn that a week had passed. Text messages flooded in: “We’re so glad you’re alive,” people told her. Taking stock of her swollen body, she wondered, how am I going to come back from this?
Her comeback took time. Barkocy was in and out of the hospital with complications, including multiple episodes of liver rejection that her team successfully managed. She also developed infections typically seen in people taking immune-suppressing medications. “With anyone who has this type of acute liver failure, it’s a lot of putting out fires to keep people improving,” explains Patrick G. Northup, MD, medical director of the adult liver transplant program.
Barkocy doesn’t mind her current regimen of 11 pills a day, blood work every four to six weeks, and twice-a-year clinic visits. Although the cause of her liver failure remains a mystery, she’s just grateful that NYU Langone, which operates the top liver transplant program in New York State, had an available bed when she needed a hepatologist and a transplant team on her case. Having an integrated health system look after every aspect of her care made for a great outcome. “They saved my life,” she says.
Today she pays it forward by running 5Ks to raise money for organ and tissue donation and speaking to driver’s ed students about persistence, resilience, and the importance of organ donation awareness. “I’m so grateful, and I’m just trying to give back,” she says.