Dr. Orrin Devinsky is spearheading research efforts into developing new epilepsy drugs.
Photo: NYU Langone Staff
At the Comprehensive Epilepsy Center, a new understanding of epilepsy’s genetic roots—and insights linking epilepsy, sleep, and memory—are giving rise to new treatments for patients.
Novel Medications Target Epilepsy’s Cellular Origins
NYU Langone researchers continue to demonstrate leadership in the development and evaluation of new epilepsy drugs. In 2018, researchers led two single-site phase II trials of ataluren for Dravet syndrome and CDKL5, expected to conclude in early 2019. Ataluren is a small-molecule medication approved in Europe for Duchenne muscular dystrophy.
Additional center research includes a single-site trial exploring the use of fenfluramine to treat CDKL5, an international trial studying ganaxolone as a treatment for CKDL5 and PCDH19, and a trial investigating the off-label use of the plant-derived supplement vinpocetine to suppress seizures in patients with a GABA receptor mutation.
“The opportunity to host these trials puts us in a unique position to vastly expand available treatments and significantly improve quality of life for individuals with epilepsy and related disorders,” says Orrin Devinsky, MD, professor of neurology, neurosurgery, and psychiatry and director of the Comprehensive Epilepsy Center.
NYU Langone researchers are working on early-stage CRISPR therapies for epilepsies caused by mutations in DHPS, SCN1A (Dravet syndrome), and CDKL5 genes; these therapies will soon move to animal testing.
The team’s additional investigations into new genetic approaches for these and other genetic disorders could have extensive impact. “We’re targeting the gene mutations that trigger these conditions,” says Dr. Devinsky. “The resulting therapies could have far-reaching efficacy for other genetic disorders, such as blood disorders and cancers.”
Studying the Links Between Sleep, Memory, and Brain Abnormalities
For individuals with epilepsy, sleep disturbances are often a major issue—poor sleep can elicit seizures, and epilepsy itself can exacerbate sleep problems. This cycle was a driving factor in integrating a sleep center into the Comprehensive Epilepsy Center, where all patients with epilepsy are screened for sleep disorders.
“The ready availability of screening data supports both our collaborative research and our targeted clinical approach,” notes the sleep center’s pediatric sleep specialist, Karen L. Lee, MD, clinical assistant professor of neurology.
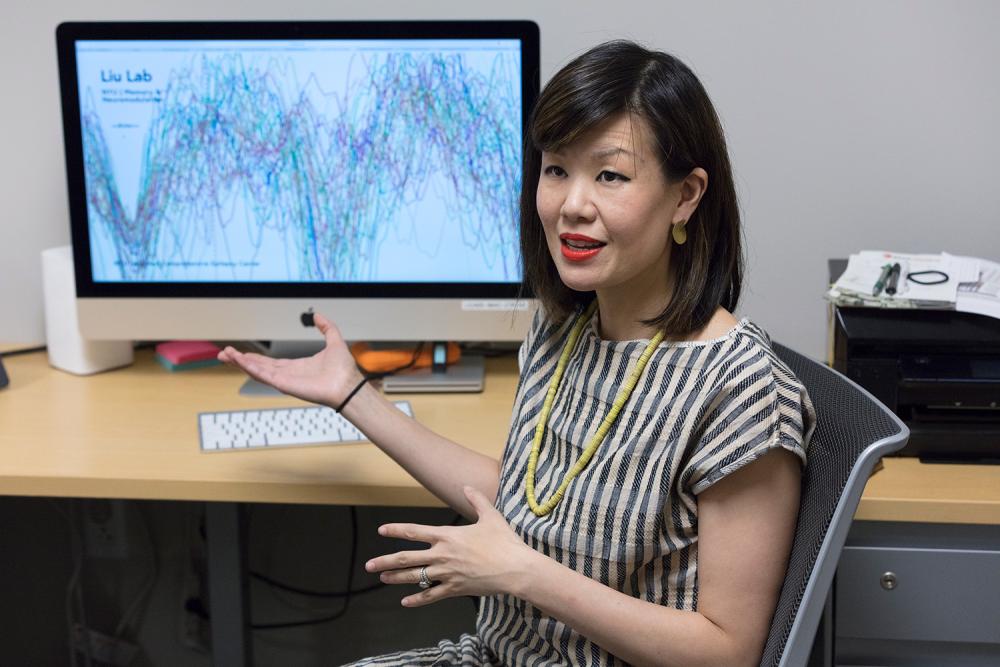
Research at the sleep center is focused on the links between epilepsy, memory impairment, and sleep. One study, supported by an National Institutes of Health Career Development (K) Award given to Anli A. Liu, MD, assistant professor of neurology, records intracranial electroencephalography (EEG) activity in patients with epilepsy as they participate in memory tasks.
Study subjects include patients with epilepsy who are undergoing invasive EEG monitoring for surgery, as well as patients with brain-implanted responsive neurostimulation devices that provide chronic EEG monitoring in an ambulatory setting. The goal is to understand how pathological electrical events such as interictal epileptiform discharges and high-frequency oscillations disrupt learning.
“Epilepsy patients commonly have impaired short- and long-term memory,” explains Dr. Liu. “If we discover that initial encoding of information is disrupted by abnormal brain waves, we could then administer treatments to inhibit these events and restore memory.”
A separate, R01 grant–funded collaboration between Dr. Devinsky, Comprehensive Epilepsy Center researchers, and György Buzsáki, MD, PhD, the Biggs Professor of Neuroscience and professor of neurology, uses techniques such as transcranial electrical stimulation and acoustic stimulation to enhance brain rhythms critical to sleep-dependent memory consolidation.
Recently, Dr. Liu’s team has been working to enhance sleep-dependent brain rhythms through a closed-loop acoustic driving approach.