PHOTO: sergunt/Getty
The kidneys of people living with systemic lupus erythematosus (SLE) are often under assault, and not all those living with the disease respond to standard treatment. A new report published online in the journal Nature Immunology online May 20 shows how tissue samples from these patients can accurately predict those who are more likely to respond to therapy. SLE is a disease marked by the attack on joints, skin, and kidneys by the body’s immune system.
“Our latest research redefines how a kidney biopsy can be used to tailor drug therapy in lupus patients,” says study co-senior investigator Jill P. Buyon, MD, the Sir Deryck and Lady Va Maughan Professor of Rheumatology at NYU School of Medicine. “Moreover, our results point to simple skin biopsy as a potential tool to track the progression of kidney damage from the disease and to tell whether treatments are working as intended or need to be changed.”
Researchers say treating lupus, which affects an estimated 1 million Americans, predominantly women, is difficult because its onset, symptoms, and progression vary significantly from person to person over time. The disorder’s origins remain unknown, although many suspect that genetic factors passed down from parents to their children as well as environmental triggers, such as sun exposure and infection, are likely responsible.
Multiple organs, including the brain and linings of the heart and lungs can be involved, the researchers add, making it harder to detect where the disease started or to predict which tissues might be affected. Existing therapies focus on immune-suppressing drugs designed to check any attack. However, these treatments are not cures and only relieve SLE signs and symptoms, such as joint pain, difficulty breathing, and low blood cell counts in some people.
For the new study, researchers analyzed the cellular profile and genetic activity of kidney and skin tissue samples from 21 people with SLE in the New York area. Most of the participants were women between the ages of 16 and 53, and of various racial backgrounds. Study participants were, at the time of biopsy, also among half of all people with SLE who experience lupus nephritis, a form of kidney inflammation that can cause lasting damage to the organ.
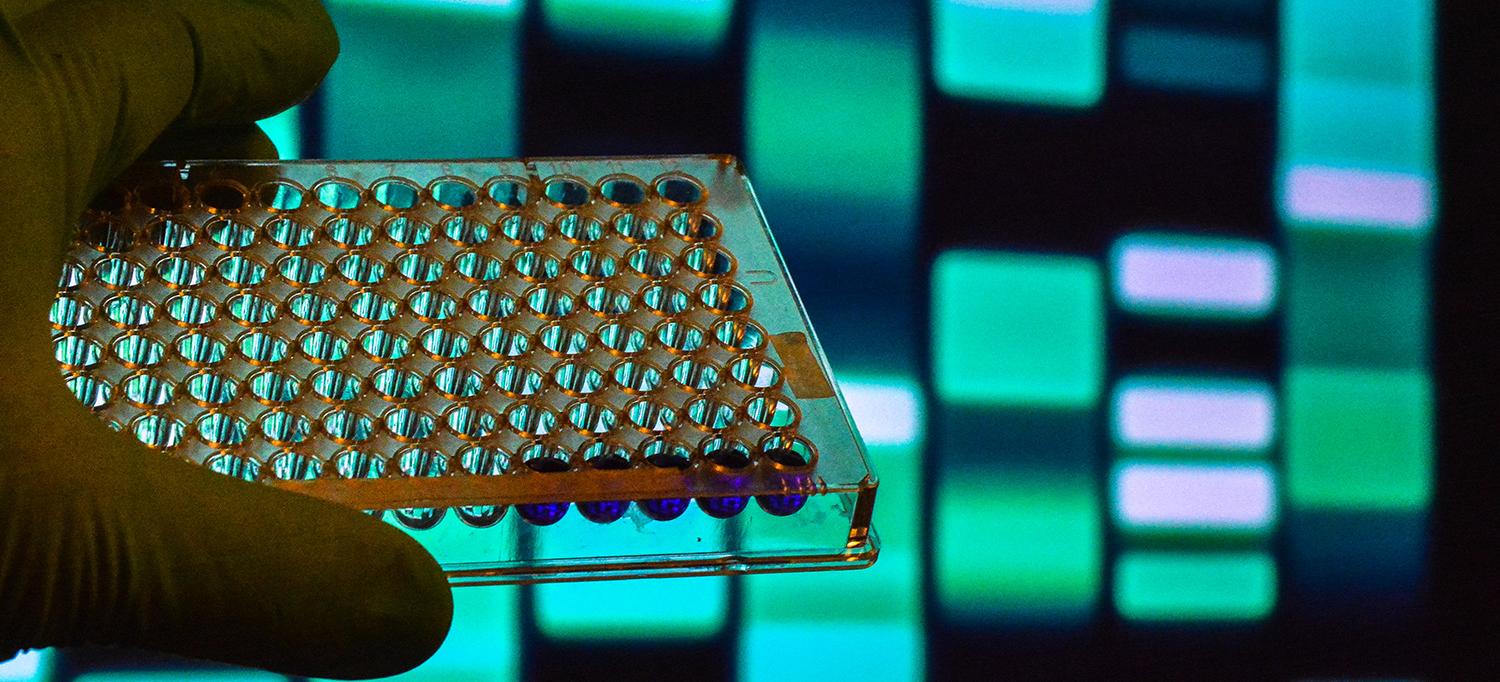
Researchers used a gene-mapping tool called scRNA-Seq that allowed them to track the action of more than 4,000 specific cells. The cell-specific biopsy profiles from people having lupus-related kidney “flares” were then compared with biopsy results from three women who did not have lupus or any other known diseases.
What the Study Revealed
Specifically, the study showed similar immune system signaling and scar-forming gene activity in kidney tubular cells affected by lupus and skin keratinocyte cells from the same participants.
Gene activity from exposure to an immune cell signaling protein, type 1 interferon (IFN), in both cell types from people with SLE increased 3.8 times and 2.5 times, respectively, when compared with biopsies from healthy women. Moreover, the increase in scar-forming gene activity in the kidney cells of people with SLE was observed in those who did not respond to therapy.
Researchers say finding similarities between cell activation in the kidney and skin is important because the skin can be more easily and repeatedly biopsied than the kidney. And since cellular changes observed in the skin closely mirrored changes involved in SLE kidney damage, sampling skin could, they say, offer clues as to what, if any, malfunction is about to occur in the kidney.
Dr. Buyon says IFN typically shows up in cells as part of the immune system response to infection and for decades has been linked to lupus. The latest study reinforces its role, as yet unexplained, in the disease.
While researchers have plans to determine the source of the IFN affecting both types of cells, they say their immediate next step is to analyze results from 160 additional patients’ kidney biopsies and as many as 400,000 different cells. They also plan to test additional skin cells, with assistance from the Judith and Stewart Colton Center for Autoimmunity, for differences between lupus patients with and without nephritis.
“If confirmed in further experiments, our findings could personalize lupus therapy based on what an individual patient’s cells are telling us about immune activity,” says Dr. Buyon, director of the Division of Rheumatology in the Department of Medicine at NYU Langone, where she also serves as director of its Lupus Center. “Moreover, this research should help shed light on the underlying biological pathways behind organ injury in lupus, the interrelated roles of kidney and skin cells, and how type 1 interferon propels this disease.”
Funding support for the study was provided by National Institutes of Health grants UH2 AR067676, UH2 AR067677, UH2 AR067679, UH2 AR067681, UH2 AR067685, UH2 AR067688, UH2 AR067689, UH2 AR067690, UH2 AR067691, UH2 AR067694, and UM2 AR067678. Additional funding support was provided by the Accelerating Medicines Partnership in Rheumatoid Arthritis and Lupus Network.
In addition to Dr. Buyon, other NYU Langone researchers involved in this study are co-investigators Peter M. Izmirly, MD; Robert Clancy, PhD; H. Michael Belmont, MD; Nicole Bornkamp, BS, MPH; and Ming Wu, MD. Additional research support was provided by study co-lead investigator Evan Der, PhD; and co-investigators Beatrice Goilav, MD; Saritha Ranabothu, MD; Mordecai Koenigsberg, MD; Michele Mokrzycki, MD; Helen Rominiecki, NP; Jay Graham, MD; Juan Rocca, MD; Nicole Jordan; Emma Schulte; James Pullman, MD, PhD; and study co-senior investigator Chaim Putterman, MD, at Albert Einstein College of Medicine in New York. Other researchers involved are study co-lead investigator Hemant Suryawanshi, PhD; and co-investigators Pavel Morozov, PhD; Manjunath Kustagi, MS; and study co-senior investigator Thomas Tuschl, PhD, at Rockefeller University in New York; Kamil Slowikowski, PhD; and Soumy Raychaudhur, MD, PhD, at the Broad Institute of MIT and Harvard universities in Boston; and Joel Guthridge, PhD; and Judith James, MD, at the Oklahoma Medical Research Foundation in Oklahoma City.
Media Inquiries
David March
Phone: 212-404-3528
david.march@nyulangone.org

