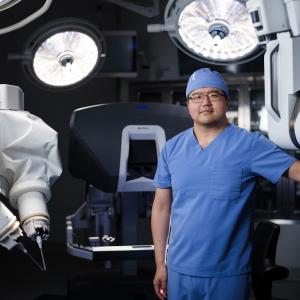
Bariatric and general surgeon Dr. Manish S. Parikh collaborates with other specialists and researchers to enhance the safety and effectiveness of various bariatric procedures.
Photo: NYU Langone Staff
Recent research led by Manish S. Parikh, MD, associate professor in the Department of Surgery at NYU Langone Health, reveals that thrombophilia is common among patients seeking laparoscopic sleeve gastrectomy (LSG) to treat obesity, potentially putting them at increased risk for portomesenteric vein thrombosis (PMVT) postoperatively. The findings suggest that extending postoperative therapy may help prevent this rare but potentially life-threatening complication.
Blood Workup Identifies Risk
PMVT is an unusual but well-known postsurgical complication in obese patients who undergo sleeve gastrectomy. However, the condition is difficult to predict because most patients do not have obvious risk factors that show up in a medical history.
In previous research, Dr. Parikh and colleagues reported that a majority of patients who developed PMVT tested positive for factor VIII—an essential blood-clotting protein. The findings prompted the investigators to order thrombophilia workups for all patients undergoing LSG and to extend chemoprophylaxis postoperatively for those with positive results.
For their latest study, the researchers recorded the prevalence of thrombophilia among 1,075 of these patients and assessed whether extended therapy was effective in reducing PMVT. Just over half tested positive for thrombophilia, and most of those (91.5 percent) showed elevated factor VIII. At the American Society for Metabolic and Bariatric Surgery’s Obesity Week, held in November 2019 in Las Vegas, the data were presented by Dr. Parikh, who is also director of bariatric surgery and chief of perioperative services at NYC Health + Hospitals/Bellevue.
Reducing Rate of Portomesenteric Vein Thrombosis Postoperatively
Patients who tested positive for thrombophilia received extended chemoprophylaxis for four to six weeks. During that time, there were 1 diagnosis of PMVT (0.1 percent) and 5 bleeding occurrences (0.6 percent). By comparison, there were 18 (0.4 percent) PMVT diagnoses and 17 (0.4 percent) bleeding episodes over 4 years before introducing routine testing. The study is currently under review for potential publication in an upcoming issue of Surgery for Obesity and Related Diseases.
The findings suggest that consideration should be given to routine thrombophilia testing (including factor VIII levels) preoperatively, combined with selective extended chemoprophylaxis (for those patients who test positive) to potentially reduce the risk of developing PMVT. However, clinicians should take into account the potential downsides of extended therapy, including longer hospital stays and patient compliance with extended prophylaxis.
“While longer-term studies are needed in this patient population, the current data suggest that routine thrombophilia testing should be considered,” says Dr. Parikh. “Combined with extended chemoprophylaxis, this strategy has the potential to significantly reduce the incidence of PMVT, which can lead to other serious complications.”