With a meticulously planned collaborative approach, backed by extensive surgical expertise, preoperative preparation, and leading-edge intraoperative monitoring, otolaryngologist Dr. J. Thomas Roland Jr. and neurosurgeon Dr. John G. Golfinos provide the best possible care for a patient with a complex tumor.
Photo: NYU Langone Staff
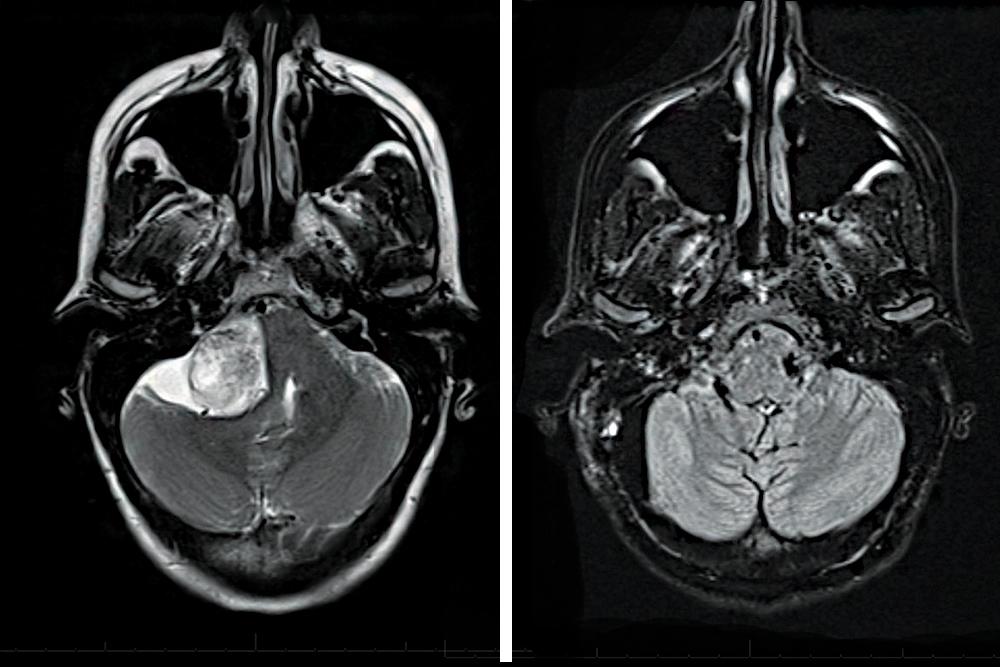
A 32-year-old patient consulted with experts at NYU Langone to evaluate her surgical options to address a large acoustic neuroma discovered despite a highly uncommon presentation. Here, a multidisciplinary team of surgeons rapidly mobilized to help her weigh the inherent surgical risks and develop a treatment plan in the context of additional complexity: The patient was 21 weeks pregnant.
As the patient’s symptoms continued to intensify, the decision was made to move forward with resection. With a carefully planned multidisciplinary approach, informed by extensive surgical expertise, preoperative planning, and advanced intraoperative monitoring, the life-threatening tumor was resected without complication, optimizing outcomes and quality of life for both the patient and her baby.
Atypical Presentation of an Aggressive Tumor
Unusual numbness and pain-like symptoms on the palate prompted the patient, herself a physician, to seek evaluation at another institution. There, an MRI revealed a 5-centimeter acoustic neuroma that was significantly compressing her brainstem. “She didn’t have the usual presentation for this kind of tumor—hearing loss and ringing in the ear,” notes J. Thomas Roland Jr., MD, the Mendik Foundation Professor of Otolaryngology and chair of the Department of Otolaryngology—Head and Neck Surgery and co-director of the Cochlear Implant Center. “Instead, she had fifth nerve symptoms because the tumor compressed the trigeminal nerve.” This delayed the diagnosis, which enabled tumor growth and added to the complexity of the treatment approach.
For this patient, the large tumor grew superior to the eighth nerve, which was entangled with the anterior and posterior inferior cerebellar arteries (AICA and PICA) distally. The tumor size, incipient hydrocephalus, and compression of the facial and trigeminal nerves would significantly increase the difficulty and duration of surgical resection. “Such complex acoustic neuroma cases are best managed with a multidisciplinary team approach combining the complementary expertise and surgical skill of two highly subspecialized surgeons, ensuring the best possible outcomes,” says John G. Golfinos, MD, associate professor of neurosurgery and otolaryngology and chair of the Department of Neurosurgery.
The patient’s pregnancy added an additional layer to the complexity of treating such a large, aggressive tumor. Though there were no guarantees that the pregnancy would survive the surgery, delaying intervention until fetal viability was contraindicated as the tumor presented life-threatening risks such as hydrocephalus and stroke if allowed to grow. Radiation was also ruled out, due to the dose requirements of such a sizable tumor.
Weighing Treatment Options with Two Patients in Mind
Together, Dr. Roland and Dr. Golfinos helped the patient weigh her options. Surgery could be delayed until fetal viability using steroid treatment, or a shunt could be placed to temporarily reduce the pressure on her brain until 36 weeks of pregnancy. The other option: they could proceed with surgery as soon as possible, despite fetal risk. If surgery were elected, the team’s advanced neurophysiologic monitoring capabilities would be critical to maximize preservation of facial nerve and other brain function during the operation. With these considerations in mind and a plan carefully crafted, the patient opted for immediate surgery, which was scheduled for later that same week.
Throughout the consult, Dr. Roland and Dr. Golfinos were transparent with the patient about the certainty of single-sided hearing loss, which occurs in about 40 percent of acoustic neuroma resections. Though the risk was unavoidable given the size and location of this patient’s tumor, the team offered unique expertise in leading-edge single-sided deafness technologies.
A Team Approach in Combination with Careful Monitoring
The patient was prepped, and an ultrasound confirmed fetal heartbeat. Intervention on the previable fetus would not be possible in case of distress, so intraoperative fetal monitoring was not elected. The team’s neuro-anesthesiologists administered neural anesthesia, avoiding fetal risks of traditional paralytic agents and enabling intrasurgical monitoring of the patient’s brain activity.
The surgical team performed the opening and exposure of the site through the mastoid, using the translabyrinthine approach. Resection of the tumor began after the stimulating probe was used to explore the posterior face of the tumor, confirming the facial nerve was not aberrantly located. Dr. Golfinos and Dr. Roland worked in tandem to debulk and dissect the tumor, freeing it from the facial nerve and the brainstem.
Using a facial nerve function measurement technique as well as traditional facial nerve monitoring, the tumor dissection was performed without complication. Neurophysiologists monitored brainstem and motor function during the procedure to confirm the tumor was resected while cranial nerves were maintained and pressure from the brainstem was relieved.
“This type of tumor stretches and thins out the facial nerve, so if you’re using traditional nerve stimulation you might incorrectly assume that the facial nerve has become dysfunctional because you are stimulating the edge of the nerve,” notes Dr. Golfinos. “If you can stimulate from the cortex and get the whole nerve stimulated, as we do, it gives you confidence that the nerve is still OK—and actually speeds up the operation.”
With the resection complete and the facial nerve stimulating well at the brainstem with robust response, the patient was sent to recovery, where postoperative ultrasound revealed a fetal heartbeat.
Complexity Navigated, Surgical Risk Rewarded
An MRI two weeks after surgery confirmed total tumor removal and a restoration of the previously compressed brainstem to its normal size. As the team had cautioned, the patient lost hearing on the right side and experienced facial weakness, which has improved over time. Her recovery has been otherwise unremarkable, and months after the operation, the team received photos of the patient’s healthy baby girl.
“Our unique collaboration between otolaryngologists and neurosurgeons offers the expertise needed to remove a tumor like this safely and completely,” says Dr. Roland. “Further, we had prepared this patient for the likelihood of hearing loss, and she knew we had the most advanced approaches needed to address her single-sided deafness. We’re continuing to work with her to restore her hearing and quality of life to the greatest extent possible, as she takes on parenthood.”