At NYU Langone, studies on schizophrenia, including those led by Dr. Esther Blessing, are exploring the effects of antidepressants and how brain structure may predict treatment response.
Photo: NYU Langone Staff
To develop improved treatments for schizophrenia—and advance a precision medicine approach to the disease—it is essential to learn how factors ranging from patient history to variations in neural circuitry shape response to medication. Researchers at NYU Langone Health are playing pivotal roles in that quest.
A New Role for Antidepressants?
One common challenge in treating schizophrenia is the recalcitrance of negative symptoms, such as apathy and anhedonia, a psychological condition characterized by the inability to derive joy in everyday pleasures. No medications have been approved for such symptoms, which often precede the onset of psychosis and may remain debilitating after it is brought under control. “It’s a big unmet need in the field,” says Donald C. Goff, MD, the Marvin Stern Professor of Psychiatry and vice chair for research in the Department of Psychiatry.
Some studies suggest that antidepressants may reduce negative symptoms in patients with chronic schizophrenia, but evidence for their efficacy has not been firmly established—and far less is known about their use in the early stages of the illness.
In March 2019, a team led by Dr. Goff published the first study investigating the use of an antidepressant for negative symptoms and subclinical depressive symptoms in first-episode schizophrenia (FES). As reported in the journal Schizophrenia Research, the multisite Depression and Citalopram in First Episode Recovery (DECIFER) Study followed 95 patients with FES who were randomized to citalopram or placebo along with clinician-determined antipsychotics over a 52-week period. All participants also received regular sessions of psychoeducation and relapse prevention.
Although the antidepressant had little effect on depression scores, negative symptoms were significantly reduced in the citalopram group compared with placebo. The effect size was greatest for patients with a duration of untreated psychosis (DUP) of more than 18 weeks compared with those with shorter DUP—effect sizes of 0.52 (medium) versus 0.32 (small). The difference reflected the fact that patients with longer DUP typically had less response to placebo, making their improvement with citalopram more striking.
“The only other treatment with known benefits for negative symptoms is folate,” notes Dr. Goff, whose research helped reveal that substance’s utility more than a decade ago. “Our study suggests that for some patients with FES, citalopram’s effects may be more robust.”
The Benefits of Brain-Derived Neurotrophic Factor
Dr. Goff’s citalopram findings grew out of his longtime research into the effects of medication on brain structure and function in schizophrenia. In 2018, he and his colleagues published a study in JAMA Psychiatry on hippocampal volume loss, which is associated with poor outcome in the disease. The team found that hippocampal volume was lower at baseline in patients with first-episode psychosis (FEP) than in healthy controls and continued to decline over an eight-week period after treatment was initiated. The degree of loss correlated with DUP and with molecular biomarkers of inflammation, oxidative stress, glial injury, and brain-derived neurotrophic factor (BDNF).
Because BDNF seemed to play a protective role, Dr. Goff reasoned, antidepressants such as citalopram—which raise BDNF levels—might help protect against hippocampal shrinkage. The new study failed to confirm that hypothesis, but it did indicate that a BDNF-enhancing drug could be clinically beneficial for patients with longer DUP. “Citalopram may allow these patients to be more responsive to psychotherapy and other kinds of psychosocial stimulation,” he explains. The medication may also serve a protective function in other brain regions—a hypothesis that Dr. Goff and his colleagues are exploring in the next phase of the study.
Finding Biomarkers to Predict Antipsychotic Response
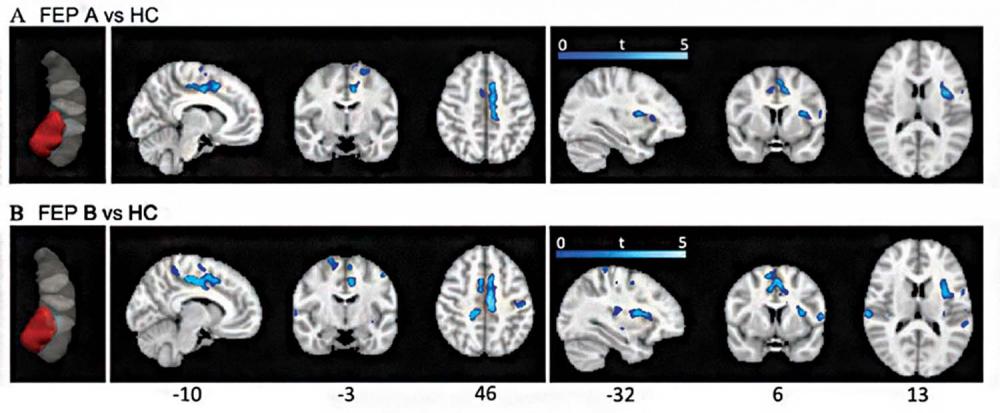
A study led by Esther Blessing, MD, PhD, assistant professor of psychiatry, further explores the role of the hippocampus in early stage schizophrenia—particularly the anterior portion of that brain structure. Published in August 2019 in Schizophrenia Bulletin, the study provides new insights into anterior hippocampal abnormalities in treatment-naive schizophrenia patients, and how antipsychotic medications affect this crucial area.
A growing body of evidence suggests that anterior hippocampal structures play a key role in ultra high–risk and FEP stages of the illness. For example, researchers have found reduced volume only in this part of the hippocampus. In rodent models of psychosis, connections are altered between the anterior hippocampus (or its animal equivalent) and certain subcortical and prefrontal regions. Yet little is known about how anterior hippocampal connectivity differs between humans with FEP and normal controls. A corollary question is whether differences in connectivity among FEP patients themselves might help explain their differing responses to antipsychotics.
To probe these mysteries, Dr. Blessing analyzed imaging data collected by Dr. Goff and his collaborators in Shanghai in a study of 61 FEP patients receiving their initial course of antipsychotics and matched healthy controls. Dr. Blessing’s analysis is the first study of functional connectivity (FC) between subregions of the hippocampus before and after medication in treatment-naive FEP patients. Imaging was conducted with resting-state functional MRI, which measures changes in blood oxygen level–dependent (BOLD) signal when the brain is not engaged in a specific task.
Dr. Blessing previously developed a data-driven method for analyzing FC that distinguishes the anterior from the posterior hippocampus. The results were clear: Compared with controls, patients with FEP had reduced anterior hippocampal connectivity with the salience network—a network of brain regions, including the insular cortex and anterior cingulate cortex, involved in identifying and filtering behaviorally relevant stimuli.
What’s more, this abnormality was corrected by antipsychotic treatment, and the pattern of clinical response to antipsychotics was predicted by a specific pattern of connectivity at baseline. “It’s currently very challenging to predict how antipsychotics will affect a given individual,” Dr. Blessing observes. “Although our findings are preliminary, they suggest anterior hippocampal FC could provide useful information for tailoring therapeutic strategies and developing more targeted treatments.”