Photo: Love Employee/Getty
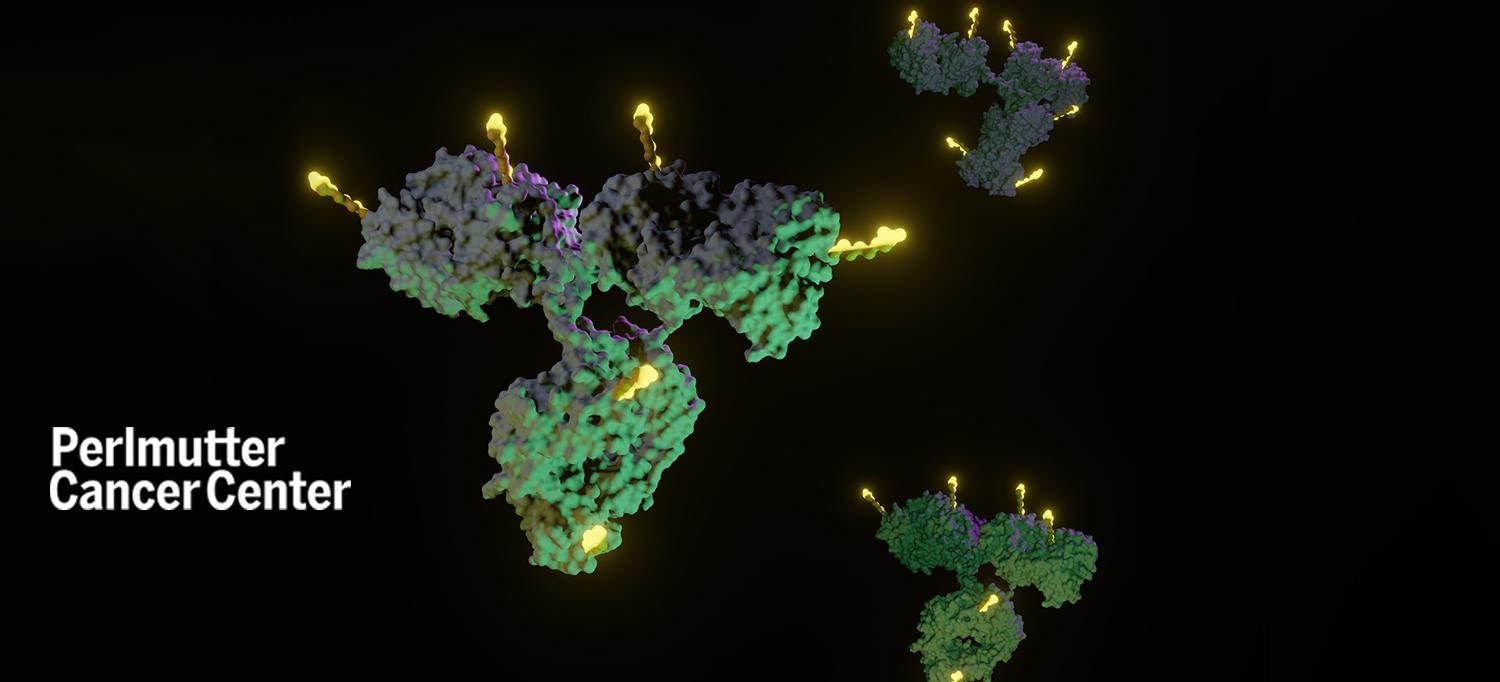
Antibody–drug conjugates—a new class of anti-cancer agent that combines a targeting antibody with a tumor-killing drug via a linker—are emerging as a new way to kill cancer cells with the goal of greater specificity and less toxicity. Two recently launched clinical trials at NYU Langone Health’s Perlmutter Cancer Center are testing antibody–drug conjugates to treat gynecologic cancers.
“Antibody–drug conjugates are the new frontier for treating cancer, and specifically gynecologic cancers,” says Bhavana Pothuri, MD, director of gynecologic oncology clinical trials at Perlmutter Cancer Center. “Antibody–drug conjugates deliver targeted cytotoxic warheads with greater specificity, and therefore we expect to see higher efficacy.”
Dr. Pothuri notes that 11 antibody–drug conjugates have been approved by the U.S. Food and Drug Administration (FDA), but to date only 2 specifically for gynecologic cancers: tisotumab vedotin for cervical cancer and mirvetuximab for platinum-resistant ovarian cancer (cancer that recurs 6 months after treatment with platinum-based chemotherapy).
Maintenance Therapy for Platinum-Sensitive Ovarian Cancer
Dr. Pothuri is leading a phase 3 clinical trial at Perlmutter Cancer Center that is evaluating an antibody–drug conjugate called XMT-1536 (upifitamab rilsodotin) as a post-platinum maintenance therapy (treatment given to help keep cancer from coming back after it has disappeared following the initial therapy) for people with platinum-sensitive recurrent ovarian cancer. XMT-1536 targets NaPi2b, a protein widely expressed in ovarian cancers but with limited expression in normal tissues.
The global multicenter trial, called UP-NEXT, is sponsored by Gynecologic Oncology Group (GOG) Partners.
In 2020, XMT-1536 received fast-track designation from the FDA for the treatment of people with platinum-resistant high-grade serous ovarian cancer who have received up to three prior lines of systemic therapy or those previously treated with four prior lines of systemic therapy regardless of platinum status.
Currently, there is no effective maintenance standard of care treatment for people with platinum-sensitive ovarian cancer who relapse and have received a PARP inhibitor or the antiangiogenesis agent bevacizumab, and some individuals are ineligible for these current maintenance options.
“We believe that XMT-1536 will prolong the progression-free survival of people with relapsed platinum-sensitive ovarian cancer,” says Dr. Pothuri, who is also a professor in the Departments of Obstetrics and Gynecology and Medicine at NYU Grossman School of Medicine and medical director of the Clinical Trials Office at Perlmutter Cancer Center.
A New Strategy for HER2-Positive Endometrial Cancer
Whitfield B. Growdon, MD, a gynecologic oncologist at Perlmutter Cancer Center, is leading a phase 1/2a first-in-human study of the antibody–drug conjugate DB-1303 for people with HER2-positive endometrial cancer.
About 60 to 75 percent of high-grade endometrial cancer tumors express some level of HER2, which is found in other human cancers, including breast, colorectal, gastric, esophageal, and ovarian. High-grade endometrial cancers have a higher recurrence rate and frequently metastasize. While anti-HER2 therapies, such as trastuzumab, have been successful in treating HER2-positive breast and gastric cancers, resistance mechanisms in HER2-positive endometrial cancer have rendered these treatments less effective. DB-1303, which combines a HER2-targeting antibody with a cytotoxic drug, may overcome the resistance mechanisms that have thwarted other HER2-targeting therapies in the gynecologic space.
The multicenter international trial is studying DB-1303 in a number of solid tumors, including breast, lung, gastric, and biliary. The trial at Perlmutter Cancer Center is part of the endometrial cancer expansion cohort, and therefore focused only on that disease site.
One of the major barriers to treating HER2-positive gynecologic cancers, including endometrial cancer, with anti-HER2 agents is that the amount of HER2 expression in these tumors tends to be lower than in other disease sites. HER2-positive breast cancers, for example, can have 10 times as many copies of the HER2 gene, compared to endometrial cancers, which might have only twice as many copies. Previous studies of DB-1303 suggest that this agent has excellent activity in low HER2-expressing tumors, which means that more people with HER2-positive endometrial cancer might derive benefit from this novel agent.
“We previously thought that anti-HER2 agents would only be effective in the 20 to 30 percent of people who overexpressed HER2,” says Dr. Growdon, who is also a member of the faculty in the Department of Obstetrics and Gynecology. “Evidence suggests that DB-1303 has excellent activity in tumors that express the range of HER2 positivity, which means that 60 to 70 percent of people with high-grade endometrial cancer will be eligible for this trial. If we can show that DB-1303 is as effective in endometrial cancer as trastuzumab was in breast cancer, this could be a supreme game changer for people with HER2-positive gynecologic cancers.”

