Photo: dzika_mrowka/Getty
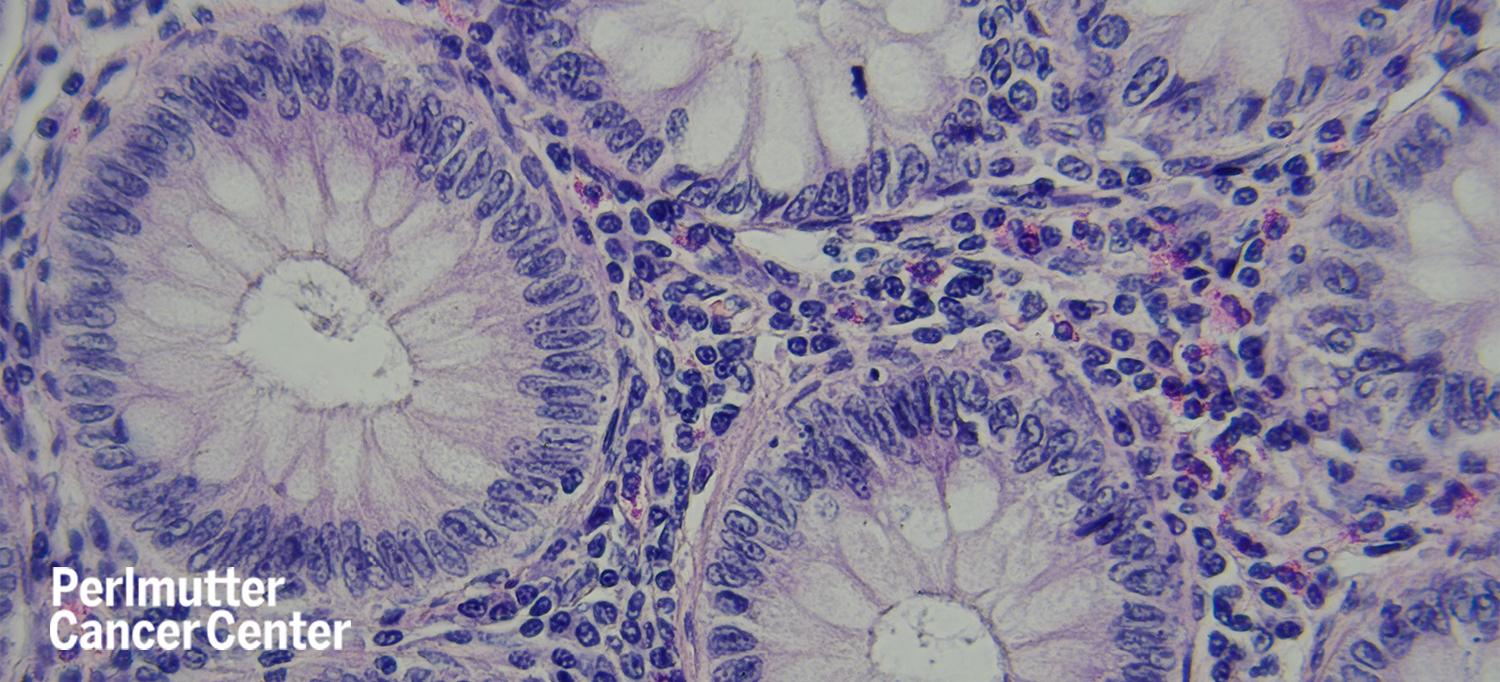
Some people with colorectal cancer who have their tumors surgically removed are at risk for a recurrence of their cancer. Chemotherapy after surgery, known as adjuvant therapy, is used to prevent recurrence, but a common side effect is neuropathy. Michael Shusterman, MD, a gastrointestinal oncologist at NYU Langone Health’s Perlmutter Cancer Center, is leading a clinical trial at Perlmutter Cancer Center at NYU Langone Hospital—Long Island aimed at using circulating tumor DNA (ctDNA) to identify which patients will benefit from adjuvant therapy and those who can safely forego additional chemotherapy.
“There is a certain percentage of people with stage 2 or 3 colorectal cancer whose cancer returns regardless of the treatment they receive,” says Dr. Shusterman, also a clinical assistant professor in the Department of Medicine at NYU Long Island School of Medicine. “We don’t know with total precision who benefits from treatment. Monitoring ctDNA is one way to try to answer that question as it is detecting residual cancer cells.”
The national phase 2/3 trial, known as CIRCULATE-US and sponsored by NRG Oncology, uses an assay called Signatera to measure the amount of ctDNA in a person’s blood after surgery. The trial, which is enrolling people with stage 2 or 3 colon cancer, is composed of two arms. In the first arm, people with low-risk stage 3 colon cancer and no detectable ctDNA will be randomized to receive either standard-of-care adjuvant chemotherapy or to have observation. This arm aims to determine if people with low risk stage 3 colon cancer and no ctDNA after surgery, whose cancer is not expected to recur, and who do not receive adjuvant therapy, have the same outcomes as people who receive additional chemotherapy.
In the second arm, people with stage 2 or 3 colon cancer who have detectable levels of ctDNA will be randomized to receive standard-of-care chemotherapy or an intensified regimen of mFOLFIRINOX (oxaliplatin, leucovorin, irinotecan, and 5-fluorouracil). People with detectable levels of ctDNA after surgery are at high risk of recurrence. However, it is not known if conventional standard chemotherapy regimens can eliminate residual ctDNA and, by extension, microscopic tumors. This arm aims to assess whether a more intensive chemotherapy regimen that is used traditionally in patients with stage 4 colon cancer can clear the ctDNA.
NYU Langone Hospital—Long Island is Perlmutter Cancer Center’s principal site for this trial, with the cancer center’s Manhattan location also enrolling patients in the study.
“This trial not only brings Perlmutter Cancer Center’s gold standard of cancer care to the community of patients with colon cancer on Long Island, but it also enables people to participate and to engage with what may be the future of colon cancer care in their own community without having to travel into Manhattan,” Dr. Shusterman says. “One of the great benefits of this trial is that it gives patients the opportunity to personalize cancer treatment and potentially reduce chemotherapy exposure.”

