At NYU Langone’s Pioneering Cardiac Catheterization Laboratory, Small Devices Deliver Big Results for Patients with Severe Blockages
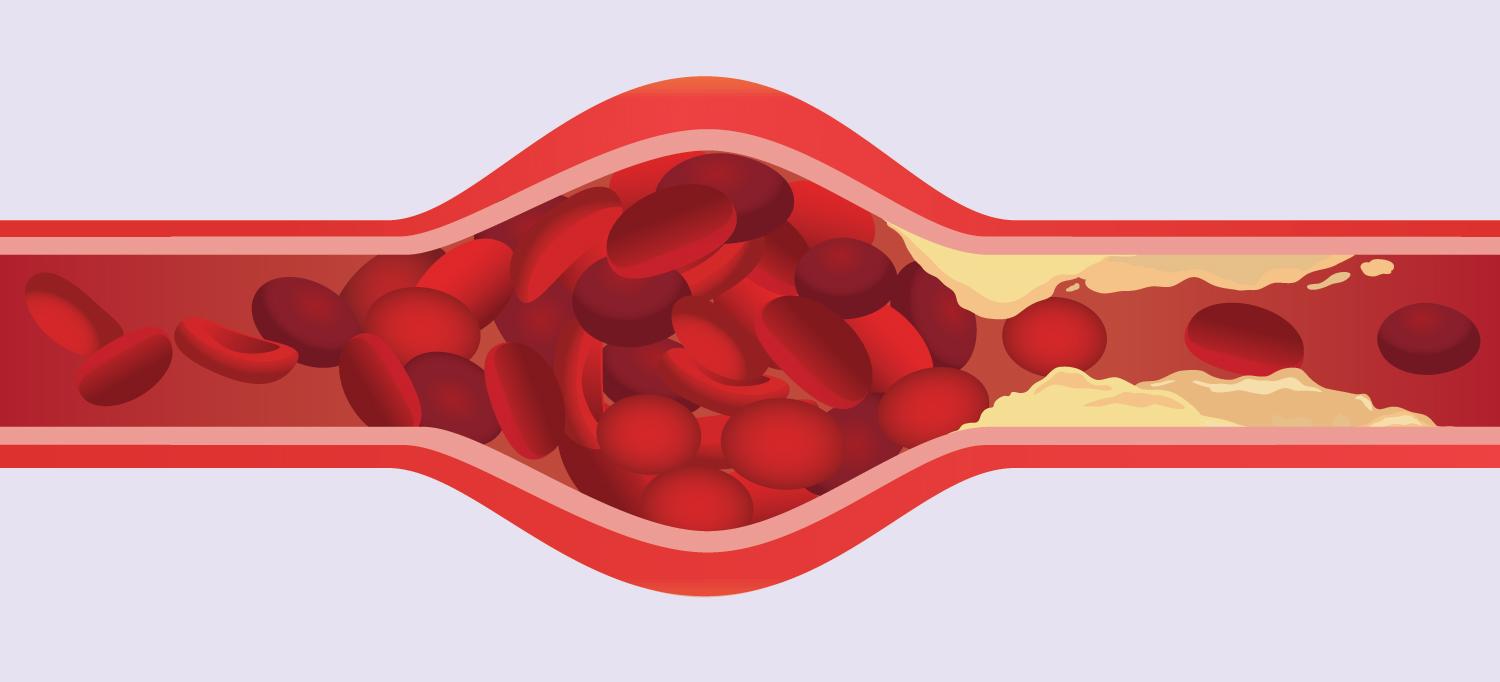
Illustration: solar22/Getty
The worst kind of arterial disease is the kind you can’t see. That’s why for decades, doctors at NYU Langone’s Cardiac Catheterization Laboratory have been pioneering techniques and tools to visualize and remove the deadly plaques of fat, cholesterol, and calcium that harden inside arterial vessels and choke off the heart’s blood supply.
The lab’s team of interventional cardiologists—among the busiest in the nation for nonsurgical interventions—can offer options to patients with even the most complex cases of heart disease. Its efforts over the years helped reduce the number of open heart surgeries in New York state by half between 2000 and 2010.
“Our field is rapidly developing,” says interventional cardiologist Craig A. Thompson, MD, who was appointed the lab’s new director in September. “Our job is to continually push the envelope to create better treatment options.”
Here are four ways NYU Langone’s Cardiac Catheterization Laboratory is saving lives.
1. Diagnosing Deadly Blockages
The Cardiac Catheterization Laboratory treats nearly 7,000 patients each year, many with heart failure. For these patients, the lab conducts thousands of diagnostic procedures to assess vital processes such as the heart’s effectiveness in pumping blood and the circulatory system’s response to drugs or devices.
Some of these assessments may follow exercise stress tests, in which patients work out on a treadmill or a stationary bike. Among the most common procedures is the angiogram, in which dye is injected into the coronary arteries to identify blockages or help surgeons prepare for bypass surgery.
2. Restoring Blood Flow
One in five patients with heart disease will develop a major blockage in a vessel delivering blood to the heart, a condition known as a chronic total occlusion. Each year, the Cardiac Catheterization Laboratory performs an estimated 2,100 coronary interventions to treat people with these obstructions percutaneously—that is, by inserting a catheter through a puncture in the skin. This noninvasive technique can serve as a vital alternative to open heart surgery and medication.
Among the lab’s arsenal of tools: balloon catheters to open blockages; tiny stents to expand arteries; and drills and lasers that pare away plaques and debris to restore blood flow.
3. Tackling the Most Complex Cases
About 10 percent of the Cardiac Catheterization Laboratory’s patients are grappling with life-threatening coronary artery disease that requires an immediate intervention to repair or widen obstructed arteries. Often, such patients have been given poor options or none at all due to the high risk for complications. They may have weakened heart muscles that require mechanical support systems to keep the heart pumping, or they may require the clearance of multiple blockages or hard-to-reach or highly calcified blockages. The lab has options for even the toughest cases.
4. Resolving Blockages in the Limbs
An estimated 2 million Americans over age 50 experience symptoms of critical limb ischemia, an advanced stage of peripheral vascular disease in which arterial blockages can threaten a leg or foot due to insufficient blood flow. The Cardiac Catheterization Laboratory performs up to 600 procedures each year to address the complications of peripheral vascular disease, including some cases that involve critical limb ischemia.
“We can treat patients in need of interventions for arterial blockages just about anywhere—in the legs, kidneys, or upper extremities,” says Dr. Thompson, “or even in the carotid artery in the neck, which is a risk factor for stroke.”
Remarkably, he says, the combined efforts of the lab’s cardiologists and NYU Langone’s bypass surgeons have saved the legs of more than 70 percent of patients with critical limb ischemia who were told by other hospitals that they needed an amputation.

