NYU Langone’s Gleaming New Kimmel Pavilion & Hassenfeld Children’s Hospital Set a New Standard for Patient Care

Image: Ennead
NYU Langone broke ground on the new Helen L. and Martin S. Kimmel Pavilion and Hassenfeld Children’s Hospital in February 2014. But in a sense, the foundation for the building—one of the most technologically integrated and digitally sophisticated inpatient facilities in the country—was laid a decade ago. As part of NYU Langone Health’s sweeping Campus Transformation plan, the information technology for the entire institution had to be reimagined and redesigned. NYU Langone has invested more than $400 million in a host of IT initiatives and systems.
“These new facilities are linchpins of our broader transformation,” notes Vicki Match Suna, AIA, senior vice president and vice dean for Real Estate Development and Facilities. “Their design has enabled us to introduce innovative digital technologies that provide the safest, most advanced, and most compassionate patient-centered care.” Many of these projects—including NYU Langone’s electronic medical record system, Epic—were implemented well in advance of Kimmel Pavilion’s debut. They modernize and streamline many patient-related activities previously performed in person or on paper.
As a new facility, the Kimmel Pavilion and Hassenfeld Children’s Hospital provided a blank slate for devising fresh ways to enhance patient-centered care. “All of these digital devices talk to each other,” explains Nader Mherabi, senior vice president, vice dean, and chief information officer. The result is a truly digital inpatient experience. “The idea is to support physicians and nurses with real-time data at the bedside, as well as their connections with other clinicians across NYU Langone and the entire health system,” adds Paul A. Testa, MD, chief medical information officer and a member of the technology leadership team.
These innovations were developed with input from clinicians and patients. They span a range of applications— from pocket-size workstations for caregivers, to robots that transport meals and linens, to surgical navigation displays in the OR. But what they share in common, notes Mherabi, is their value to patients, their families, and caregivers.
“Our goal was to push the boundaries of the digital frontier,” says Mherabi. “But we’ve been very careful not to implement technology for technology’s sake. Every decision was guided by what’s right and best for the people we serve.
We’re empowering patients with personalized, convenient, state-of-the-art tools that enhance their hospital experience before, during, and after their stay.”
If This Wall Could Talk—and It Does
Even its name—MyWall—speaks volumes about the digital communications hub that’s integral to every patient room in the Kimmel Pavilion and Hassenfeld Children’s Hospital. The full-service electronic system empowers patients by allowing them to customize their personal space. From a bedside tablet or remote control, the patient commands the content of a 75-inch-wide high-resolution monitor. MyWall offers an impressive array of conveniences and amenities, introduced to new patients upon arrival in a welcome video.
At the touch of a screen or button, patients can get to know their care team, review test results with physicians, ask questions about their treatment plan, view educational videos, and order meals according to the prescribed diet. They can also transcend the confines of a hospital room by Skyping with family and friends, surfing the web, and watching TV or movies. MyWall gives patients a say in their environment, allowing them to adjust the room’s temperature, lighting, and window shades to their own preferences. They can further enhance the ambience by displaying digital artwork or uploading personal photos. In children’s rooms, a video game player with parental controls is integrated into the system.
Automating the Legwork
Patients may never glimpse the mobile robots that roam the service corridors, but these behind-the-scenes utility-cabinets-on-wheels will benefit them in unseen ways. A fleet of 31 autonomous robots transport linens, supplies, and meal trays; remove medical waste; and deliver medications to pharmacy hubs on each patient floor, freeing up staff and caregivers to focus on the needs of patients.
The robots use lasers to build a detailed three-dimensional map of their environment, and infrared and ultrasonic sensors to avoid collisions. As they navigate hallways, they communicate via Wi-Fi with elevators and automatic doors, as well as passersby. The well-mannered machines cede the right of way to human coworkers, announce their arrival, and issue a warning before backing up. On a weekly basis, each robot traverses many miles, sparing the staff lots of time and legwork.
Smarter, Safer Bed Rest
Most hospital beds are adjustable, but some modifications, such as lowering the bedrails or elevating parts of the bed at a steep incline, can be harmful to patients who are at risk for falls or whose range of motion is restricted by wounds, back injuries, or other medical issues.
The new iBed system addresses these concerns with a host of sophisticated electronic features that enhance patient safety and comfort. Communicating wirelessly with Epic, NYU Langone’s electronic health record system, the iBed conforms to prescribed guidelines for the patient’s risks and restrictions. In addition to automatically measuring the patient’s weight, the iBed issues critical alerts, notifying caregivers when patients leave their bed and when it’s time to reposition them to help prevent pressure sores or ventilator-associated pneumonia.
A Personalized Micropharmacy
Managing and distributing medications to hundreds of patients who are on multiple prescriptions that may change over time is one of the most daunting challenges—and most critical responsibilities—for any hospital. NYU Langone makes this process faster, safer, and more efficient with the use of the digital medication drawer, the first technology of its kind implemented at any hospital in the US. This medication storage system syncs prescriptions and dosages with the patient’s electronic medical record, customizing and updating its inventory.
A kind of micropharmacy, the digital medication drawer is located just outside every patient’s room. Nurses access the locked system by using a fingerprint scanner, and use another scanner to read the unique barcode assigned to each patient—the same one that appears on the patient’s hospital-issued wristband. As medications are stocked, retrieved, and administered, they are checked and rechecked to ensure that the right ones reach the right patient at the right time.
MRI in the OR
During an operation, images from an MRI can provide the surgeon with critical information, confirming the success of the procedure in real time, indicating where additional surgery is needed, or even changing the course of the operation. Obtaining that information, however, would require the patient to be transported to the nonsterile environment of a radiology suite, raising the risk of infection and extending the length of the operation.
At the Kimmel Pavilion and Hassenfeld Children’s Hospital, MRI equipment is available in the OR itself, where it can be positioned around the patient and the surgical bed. Called intraoperative MRI, or iMRI, this technology is particularly valuable to neurosurgeons because it enables them to differentiate tumor tissue from normal tissue, minimize disturbance of critical regions, and make adjustments to their approach without moving the patient.
A Handheld Workstation
The stream of patient-related information that doctors and nurses must navigate as they move from patient to patient within a hospital is not only enormous, but virtually continuous. An iPhone is a valuable resource for managing the flow, and NYU Langone has designed a suite of innovative applications that bring the device to another level. The Clinical Mobile Companion, installed on 2,600 iPhones, incorporates a unique set of tools that enable the patient’s care team to stay on top of urgent developments.
From the palms of their hands, nurses can access the patient’s medical record, monitor vital signs, review lab results, send secure text messages, receive alerts from patient-monitoring devices, and scan identification barcodes on medication containers and wristbands. The augmented iPhones are equipped with long-life batteries to ensure all-day service.
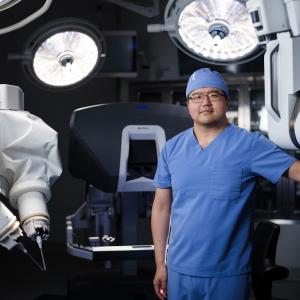
Visuals Give Surgeons a Better View
To help surgeons plan a procedure, monitor its progress, and modify their approach in response to changing situations, ORs are typically equipped with numerous display screens. So much clinical and visual data bombards the surgical team, however, that unless it’s integrated, it can be difficult to obtain a high-level overview of the patient’s status and the procedure in progress. Enter the OR Audio Visual Management System, a centralized information hub installed in the pavilion’s 30 operating rooms and image-guided labs.
The system gathers a wealth of critical information and images, and displays it on as many as eight large monitors. The largest ones help the surgeon visualize, navigate, and evaluate even the most complex procedures in real time. The surgeon can call up multiple live video feeds from a variety of imaging equipment, and can record, enhance, and interact with the images. The system can also draw information from the patient’s electronic medical record and allow the surgeon to video-consult directly with a pathologist. Even before an operation begins, the system goes to work, projecting soothing nature scenes on the monitors before anesthesia is administered to the patient.
Clinical Snapshots of Critical Patients
When a nurse or physician checks on a patient in a critical care unit, getting up to speed on the patient’s status can take time away from interacting with the patient and their family. To make the most of a caregiver’s time, each of the 170 patient rooms devoted to critical care at the Kimmel Pavilion and Hassenfeld Children’s Hospital is equipped with a 42-inch-wide wall-mounted touchscreen monitor that provides an instant overview of the patient’s current condition. A physician or nurse can bring up real-time data about the patient, viewing it in greater depth or over a longer time frame if desired. On the same high-resolution touchscreen, the care team can also huddle together and review radiology images.