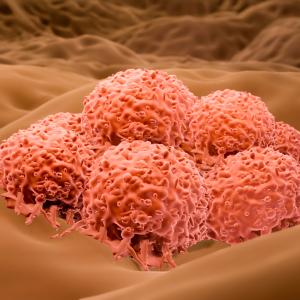
Melanoma cells growing in culture.
Photo: Karsten Moran
NYU Langone’s Ronald O. Perelman Department of Dermatology has received a 5-year, $11 million grant from the National Cancer Institute (NCI) to design tools that predict whether therapies that help the immune system fight cancer will be effective in treating melanoma.
While such immunotherapies have shown promise in treating many types of cancer, there is an urgent need for more tests to detect biomarkers, which can help doctors tailor care by predicting both a patient’s response to a treatment and his or her risk of immune-related side effects.
This is NYU Langone’s first grant to be funded by the NCI’s P50 Specialized Programs of Research Excellence (SPORE), which promote interdisciplinary research to help research findings move quickly from the laboratory to the patient. This achievement builds upon the recent accomplishment of NYU Langone’s Perlmutter Cancer Center, which earned Comprehensive Cancer Center designation by the NCI as one of 50 such cancer centers nationwide.
NYU Langone’s melanoma SPORE focuses on “checkpoints”—sensors on immune cells that turn them off when they receive the right signal. While designed to attack invading viruses and bacteria, immune cells also recognize tumors as abnormal, but cancer cells hijack checkpoints to turn off these responses. Checkpoint inhibitors are a type of immunotherapy that counter this effect, but scientists need more detailed guidance on how to use them to treat metastatic cancer, and as a secondary treatment, known as adjuvant treatment, for particular types of cancer.
“The U.S. Food and Drug Administration’s approval of immunotherapies in this clinical context has led to an increase in the use of these treatments with expansion of adjuvant clinical trials to other cancers,” says Seth J. Orlow, MD, PhD, the Samuel Weinberg Professor of Pediatric Dermatology, professor of cell biology and pediatrics, and chairman of the Ronald O. Perelman Department of Dermatology. “Identifying biomarkers predictive of benefit and toxicity is critical and timely, and promises to have broad applicability.”
The SPORE consists of projects that assess the clinical relevance of proposed biomarkers, in some cases within an investigator-initiated clinical trial. “NYU Langone’s broad patient base and expertise in biomarker identification, as well as its experience with clinical trials of immune checkpoint inhibitors, make it particularly well-suited to achieve these objectives,” Dr. Orlow says.
The program will be led by co-principal investigators Iman Osman, MD, professor in the Ronald O. Perelman Department of Dermatology, professor in the Departments of Medicine and Urology, and associate dean for translational research support, and Jeffrey S. Weber, MD, PhD, the Laura and Isaac Perlmutter Professor of Oncology in the Department of Medicine and deputy director of Perlmutter Cancer Center.
Drs. Osman and Weber, who co-direct Perlmutter Cancer Center’s Melanoma Research Program, have complementary expertise in developing immunotherapies and biomarkers. For example, in 2002, Dr. Osman established NYU Langone’s Interdisciplinary Melanoma Cooperative Group, which currently includes 24 investigators from 10 different departments. The program has since collected more than 80,000 blood and tissue specimens, as well as clinical information from more than 4,000 patients, an unparalleled resource for the study of melanoma biology and its diverse outcomes.
Dr. Weber has led many clinical trials—some of which have changed clinical practice—using checkpoint inhibitors, tumor-infiltrating lymphocytes, and other agents to boost anti-cancer immunity, including an international clinical trial that uncovered the immune checkpoint inhibitor nivolumab’s superiority in late-stage melanoma, and another trial that established its utility as adjuvant therapy after surgical resection.
“This SPORE grant is a well-earned recognition of the dynamic translational research program that our melanoma group has developed,” says Benjamin G. Neel, MD, PhD, professor of medicine and director of Perlmutter Cancer Center. “Drs. Osman, Weber, and the melanoma program investigators will apply their strengths to solve pressing needs in the melanoma field which can be extended to the increasing number of cancers treated with immune checkpoint inhibitors.”