Ozzie Wade was born with half a heart. He was also born a fighter. Read about his heroic resilience and the remarkable surgical interventions that saved his life.

Hannah Davis Wade with her husband, Tom, and their 15-month-old son, Ozzie, who was successfully treated at NYU Langone for “half a heart” syndrome.
Photo: Brad Trent
Pregnant? Hannah Davis Wade felt the telltale signs of hunger and nausea simultaneously, yet how could that be? She and her husband, Tom, had stopped in vitro fertilization treatments months earlier, discouraged after a series of miscarriages and a full-term stillbirth.
So the surprise pregnancy brought as much fear as joy. At 16 weeks, a routine ultrasound showed a serious problem: a complex congenital heart defect known as hypoplastic left heart syndrome (HLHS). Dubbed “half a heart,” the condition leaves the left side of the heart so underdeveloped that it can’t effectively pump blood to the rest of the body.
Heart malformations are the most common congenital defects, affecting nearly 1 percent of births in the United States, but HLHS is rare, found in only 1 out of 4,344 newborns. Once untreatable, HLHS is now managed with three reconstructive surgeries—usually performed at birth, 3 to 6 months of age, and 2 to 3 years—that reroute blood flow to provide adequate circulation.
“We’d lost one baby and couldn’t bear to lose another,” Hannah explains. But when she and her husband met with Achiau Ludomirsky, MD, pediatric cardiologist at Hassenfeld Children’s Hospital at NYU Langone, they found the strength to go forward.
“You can do this,” he told the couple. “People with this condition survive and thrive.”
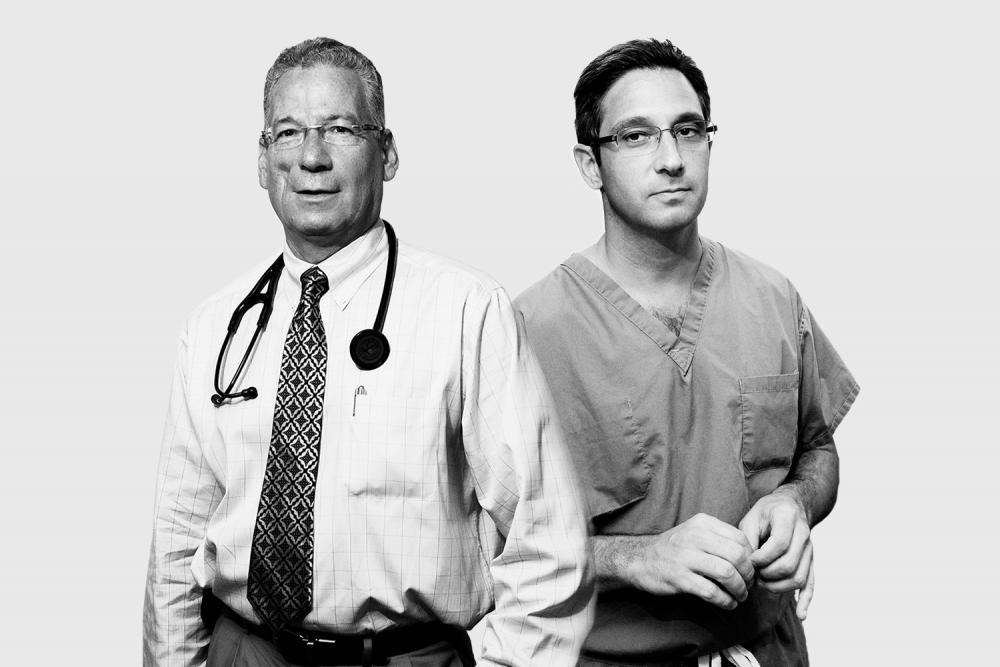
The couple also found comfort in knowing that their baby couldn’t be in better hands. Their surgeon, Ralph Mosca, MD, chief of the Division of Pediatric and Adult Congenital Cardiac Surgery, is one of the world’s top specialists. Renowned for his skill and speed—a vital asset because the infant is connected to a heart-lung bypass machine in the operating room—he has performed more than 6,000 open heart surgeries, including many complex cases.
Ozzie Wade was born on August 22, 2017, at a mere 4 pounds, 8 ounces. His parents held him for a blissful fleeting moment before a second, unexpected birth defect became apparent. Connected to a ventilator prior to planned heart surgery, Ozzie’s left lung blew up like a balloon. Unable to expel air, he fought for his life. Pediatric surgeon Jason C. Fisher, MD, prepared for an emergency lobectomy, removing about one-third of Ozzie’s lungs, which in time would grow to fill the empty space.
To make an appointment, visit the Pediatric Congenital Heart Program.
Ozzie still needed life-saving surgery on his heart as soon as possible, but the combination of compromised heart and lungs made the situation dire. The challenge of keeping him alive fell to Sujata Chakravarti, MD, director of the Congenital Cardiovascular Care Unit. With medications, a ventilator, and the power of human touch, she and her team helped Ozzie get strong enough for the first cardiac repair.
“Ozzie’s recovery from the lung surgery proved he was a fighter,” says Dr. Mosca, who created a “new” aorta and connected it to the right ventricle. “It’s one of the riskier things I do,” he acknowledges. “The baby’s heart is the size of a walnut, and the aorta—1.5 millimeters wide—is like a strand of spaghetti. There’s no room for error. No second chance to get it right.”
On September 21, 2017, Ozzie emerged from the six-hour procedure with a heart that pumped blood to his body through the right ventricle. While fully and partially oxygenated blood still comingled—to be remedied with a later surgery—the redesign gave Ozzie an immediate boost. Within two weeks, he shed all the machines and monitors, drank from a bottle, and prepared to go home.
“There’s only one word for that,” says Dr. Ludomirsky. “Miracle.”