PHOtO: GETTY/Andrew Brookes
Experiments in mice have shown early success in vaccinating them against potentially deadly bacterial infections, such as methicillin-resistant Staphylococcal aureus, or MRSA, the strain resistant to most drug treatments.
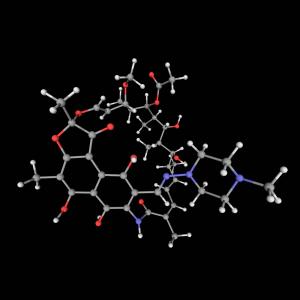
The new vaccination strategy, developed by researchers at NYU Grossman School of Medicine, targets toxic molecules released by all staphylococcal bacteria, called leukocidins, rather than directly targeting the bacteria.
Attempts to develop a staphylococcal vaccine have so far failed, researchers say, in part because leukocidins kill immune system cells, or leukocytes, needed by the immune system to fight the infection and whose production is triggered by a vaccine. As a consequence, these bacteria release leukocidins to evade not only an immediate immune cell attack, but also to prevent the infected host, whether human or mouse, from developing any long-term immunity through antibodies, which are also produced by leukocytes.
Now, a new study published online June 30 in the Journal of Experimental Medicine finds that 70 percent of mice given the experimental vaccine targeting the leukocidins survived infections with the bacterium. By contrast, no infected mice survived without the vaccine.
Previous work by the same research team found that mice could survive infection with staphylococcal bacteria whose leukocidins had been genetically modified to lose their toxic effects. These nontoxic leukocidins formed the basis of the experimental vaccine.
“Our study provides a roadmap for developing an effective vaccine against all staphylococcal infections, especially MRSA,” says study senior investigator Victor J. Torres, PhD, the C.V. Starr Professor of Microbiology in NYU Langone’s Department of Microbiology. “This strategy is based on maximum disarmament of the bacterium’s ability to kill all types of immune system cells.”
“By targeting the toxins released by the bacteria, our experimental vaccine not only stops the bacteria from killing neutrophils, a key type of leukocyte the immune system uses to destroy the invading pathogen, but also defends other leukocytes, such as T cells and B cells, needed to provide long-term protection from future infection,” says Dr. Torres.
Among the key study results was that mice repeatedly infected with toxin-releasing staphylococcal bacteria demonstrated an immune response to the infection, producing antibodies to both the bacteria and its leukocidins. However, mice infected with bacteria engineered to not produce the toxins had twice as many antibodies targeting the bacteria, showing a much stronger immune response when the toxins were absent. This heightened immune response is what researchers say led them to target leukocidins as the best possible means of giving those infected the “upper hand” in fighting the bacterium.
Dr. Torres cautions that a commercially available antileukocidin vaccine is years away. The next step for his team is to conduct clinical trials to investigate whether humans vaccinated against the toxins show a similar toxin-specific immune response as seen in the mice.
He says investigators also want to find out if the same antitoxin effects occur for any of the hundreds of other molecules released during staphylococcal infections. Dr. Torres says a “foolproof” vaccine against the bacteria, including MRSA, will likely involve targeting more than just its leukocidin toxins.
The latest United States estimates are that more than 119,000 people suffered from staphylococcal bloodstream infections in 2017, leading to nearly 20,000 deaths.
Funding support for the study was provided by National Institutes of Health grants T32 AI007180, R01 AI105129, R01 AI099394, R01 AI133977, HHSN272201400019C, R01 HL125816, and P30 CA016087. Additional funding support came from the Judith and Stewart Colton Center for Autoimmunity and the Drs. Martin and Dorothy Spatz Charitable Foundation. Dr. Torres stands to benefit financially from his patent interests with Janssen Biotech, Inc., in Raritan, NJ, the terms and conditions of which are being managed in accordance with the policies of NYU Langone.
Besides Dr. Torres, other members of the NYU Langone team are study lead investigator Kayan Tam, PhD; and study co-investigators Keenan Lacey, PhD; Joseph Devlin, BA; Maryaline Coffre, PhD; Alexis Sommerfield; Rita Chan; Aidan O’Malley; Sergei Koralov, PhD; and P’ng Loke, PhD.
Media Inquiries
David March
Phone: 212-404-3528
david.march@nyulangone.org