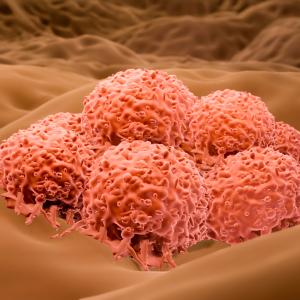
Genetic testing of tumor and blood fluid samples from people with and without one of the most aggressive forms of skin cancer has shown that two new blood tests can reliably detect previously unidentifiable forms of the disease.
Researchers at NYU Langone Medical Center and its Perlmutter Cancer Center, who led the study, say having quick and accurate monitoring tools for all types of metastatic melanoma, the medical term for the disease, may make it easier for physicians to detect early signs of cancer recurrence.
The new blood tests, which take only 48 hours, were developed in conjunction with Bio-Rad Laboratories in Hercules, California. Currently, the tests are only available for research purposes.
The new tools are the first, say the study authors, to identify melanoma DNA in the blood of patients whose cancer is spreading and who lack defects in either the BRAF or NRAS genes, already known to drive cancer growth. Together, BRAF and NRAS mutations account for more than half of the 50,000 cases of melanoma diagnosed each year in the United States, and each can be found by existing tests. But the research team estimates that when the new tests become available for use in clinics, the vast majority of all melanomas will be detectable.
“Our goal is to use these tests to make more informed treatment decisions and, specifically, to identify as early as possible when a treatment has stopped working, cancer growth has resumed, and the patient needs to switch therapy,” says senior study investigator and dermatologist David Polsky, MD, PhD.
Dr. Polsky presented his team’s latest findings at the annual meeting of the American Association for Cancer Research on April 2 in Washington, D.C.
The new tests, says Dr. Polsky, the Alfred W. Kopf, MD, Professor of Dermatologic Oncology at NYU Langone and director of its pigmented lesion section in the Ronald O. Perelman Department of Dermatology, monitor blood levels of DNA fragments, known as circulating tumor DNA (ctDNA), that are released into the blood when tumor cells die and break apart. Specifically, the test detects evidence of changes in the chemical building blocks, or mutations, of a gene that controls telomerase reverse transcriptase (TERT), a protein that helps cancer cells maintain the physical structure of their chromosomes.
Dr. Polsky says the detected changes occur in mutant building blocks, in which a cytidine molecule in the on–off switch for the TERT gene is replaced by another building block, called thymidine. Either mutation, C228T or C250T, results in the switch being stuck in the “on” position, helping tumor cells to multiply.
According to Dr. Polsky, the blood tests may have advantages over current methods for monitoring the disease because the tests avoid the radiation exposure that comes with CT scans, and the tests can be performed more easily and more often.
The Bio-Rad tests, once clinically validated, are also likely to gain widespread use quickly, he says, because his previous research had shown that similar blood tests for BRAF and NRAS mutations worked better in identifying new tumor growth than existing blood tests for the protein lactate dehydrogenase. Lactate dehydrogenase levels may spike during aggressive tumor growth, but can also rise as a result of other diseases and biological functions.
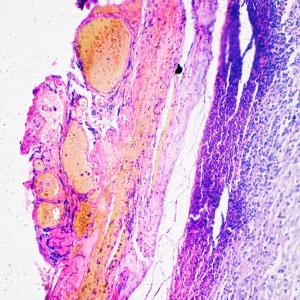
As part of the ongoing study, researchers checked results from the new tests against 10 tumor samples taken from NYU Langone patients diagnosed with and without metastatic melanoma. They also tested four blood plasma samples—the liquid portion of blood—from NYU Langone patients with and without the disease. Blood test results matched correctly in all cases known to be either positive or negative for metastatic melanoma. Successful detection occurred, they say, for samples with as little as 1 percent of mutated ctDNA in a typical blood plasma sample of 5 milliliters. Meanwhile, TERT mutations were absent in tests of normal blood plasma and tonsil tissue.
Dr. Polsky says further study of the new blood tests are planned to gauge their use in monitoring progression of the aggressive cancer, and to more quickly determine when switching to an alternative therapy is warranted, as well as whether the tests can used to detect other types of cancer, such as brain tumors, that also have TERT mutations.
Funding support for the study was provided by National Cancer Institute grant R21 CA198495, with in-kind support from Bio-Rad, which provided chemical supplies.
Besides Dr. Polsky, other NYU Langone and Perlmutter Cancer Center researchers involved in the study were lead study investigators Broderick Corless, BS, and Gregory Chang, MBA; and study co-investigators Mahrukh Sayeda, MS, and Iman Osman, MD. Additional research support was provided by study co-investigators Samantha Cooper, PhD, and George Karlin-Neumann, PhD, at Bio-Rad Laboratories.
Media Inquiries
David March
Phone: 212-404-3528
david.march@nyumc.org