Pre-Biopsy MRI May Help Avoid Overtreating Low-Grade Cancer

A study led by NYU Langone’s Dr. Samir Taneja shows the risks and benefits of prostate cancer detection by MRI-guided approaches.
Photo: NYU Langone Staff
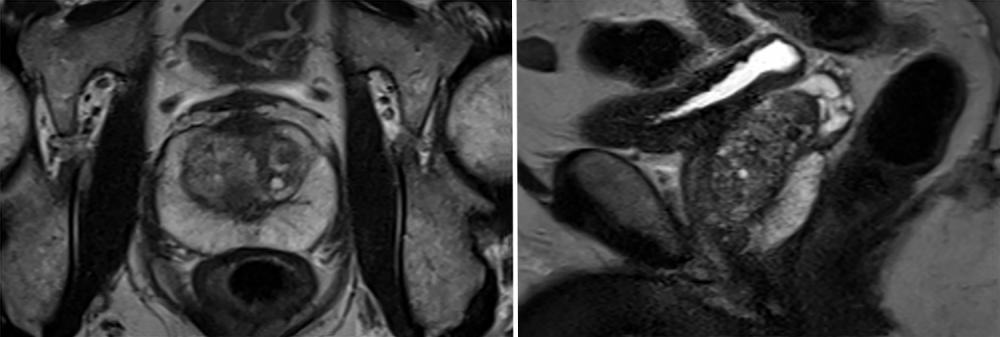
Use of MRI in men for whom there is clinical suspicion of prostate cancer, followed by MRI-targeted prostate biopsy, has been shown to improve detection of clinically significant prostate cancers warranting therapy. Additionally, its use reduces detection of low-risk cancer unlikely to harm, thereby potentially avoiding unnecessary biopsies in men not likely to have significant cancers. Pre-biopsy MRI can also reduce over-detection and subsequent overtreatment of low-grade cancers.
An influential multicenter study, dubbed the PRECISION trial, compared MRI-targeted versus standard systematic biopsy in 500 men with elevated prostate-specific antigen (PSA) levels who had not previously had a biopsy. Among men randomized to MRI-targeted biopsy, only those with intermediate to very high suspicion for cancer, based on PI-RADS (Prostate Imaging Reporting and Data System) scores of 3 or higher, were recommended for biopsy.
As a result, just over one quarter of men avoided a biopsy altogether. Further, compared with standard biopsy, MRI-guided biopsy detected more clinically significant cancer and less low-grade cancer. However, because not all men in the trial were biopsied, there remains uncertainty around the number of cancers that were missed in men receiving only MRI-targeted biopsy.
To demonstrate the generalizability of the PRECISION findings, a multidisciplinary investigative team at NYU Langone sought to apply the PRECISION biopsy strategy to an institutional study in which all patients had MRI-targeted and systematic biopsy. The study, published October 7, 2020, in The Journal of Urology, was led by Samir Taneja, MD, the James M. Neissa and Janet Riha Neissa Professor of Urologic Oncology and vice chair in the Department of Urology at NYU Langone. Dr. Taneja is also a professor in NYU Langone’s Department of Radiology, a professor of biomedical engineering at NYU Tandon School of Engineering, and leader of the Genito-Urologic Program at Perlmutter Cancer Center. He is also co-director of the Smilow Comprehensive Prostate Cancer Center and director of the Division of Urologic Oncology. The study was performed in collaboration with first author Zachary Feuer, MD, the primary authors of the PRECISION study, and the PRECISION study group.
According to the findings, application of the PRECISION strategy resulted in cancer detection and biopsy avoidance rates in 629 patients receiving diagnostic biopsy at NYU Langone as similar to those reported in the original PRECISION trial. Application of the strategy avoided biopsy in 28 percent of men with nonsuspicious MRI and reduced low-grade cancer detection by 60 percent, while also missing 19 percent of clinically significant cancers.
PRECISION Strategy Avoids Detection of Low-Risk Disease
Missed clinically significant cancers in men enrolled in the NYU Langone study were most often smaller volume and lower risk (typically <6 mm or Gleason grade 2), compared with those cancers identified on biopsy, the investigators noted.
“Clinically significant cancers we miss are most often small and minimally aggressive as compared to cancers found on MRI targeting,” says Dr. Taneja, the study’s senior investigator. “This calls into question the concern of missing such cancers as they may carry a lower likelihood of harm to the patient if untreated.”
Small or low-risk cancers may ultimately be detected in clinical follow-up if patients’ PSA levels become concerning, adds Dr. Taneja.
One limitation of the study is that only those perceived to be at higher clinical risk had a biopsy, while some with low-risk MRI (PI-RADS 1 or 2) did not, researchers note. As a result, it’s likely that the percentage of clinically significant cancers missed could be substantially lower than 19 percent if all men with low-risk MRI were biopsied.
Diagnostic Dilemma for Urologists
The PRECISION trial demonstrates that use of pre-biopsy MRI risk stratification, followed by MRI-targeted biopsy alone in men with PI-RADS scores of 3 or higher on MRI, results in increased detection of clinically significant cancer and decreased detection of low-risk cancers, relative to systematic biopsy alone, the investigators conclude. However, they note that the NYU Langone cohort findings were more in line with subsequent large studies showing that clinically significant cancer detection did not differ between MRI-targeted and systematic biopsy, but also that the combination of both improved detection of higher-risk cancers significantly.
“There is no question that MRI-targeted biopsy has dramatically improved our detection pathways. Through a combination of MRI and markers, we are able to greatly improve our ability to distinguish clinically significant cancers,” says urologic oncologist Stacy Loeb, MD, a professor in the Departments of Urology and Population Health at NYU Langone and a member of Perlmutter Cancer Center.
The NYU Langone study findings additionally suggest that cancer identified on systematic but not MRI-targeted biopsy is in many cases reflective of biopsy targeting error, which may be related to either technique or learning curve, says co-author Andrew B. Rosenkrantz, MD, professor of radiology and urology and director of prostate imaging at NYU Langone.
“The negative predictive value of MRI for clinically significant prostate cancer varies with biopsy intensity, disease prevalence, and radiologist experience,” says Dr. Rosenkrantz. “Our results, when applying the PRECISION strategy, are heavily influenced by radiology and biopsy experience. At NYU Langone, we have observed a negative predictive value of 98 percent.”
Ultimately, the findings point to a diagnostic dilemma for urologists, notes Dr. Taneja. “By applying the PRECISION biopsy strategy, we avoid detection of low-grade cancers, which is desirable, but we risk missing a smaller subset of clinically significant cancers, which is undesirable,” he explains. “Because the missed clinically significant cancers are small and generally lower risk, this may be a reasonable trade-off to avoid over-detection, but that’s a decision that individual physicians must make.”
Disclosures: Samir Taneja, MD, receives consulting fees from Trod Medical, Francis Medical, Insightec, and Janssen; is a scientific investigator for MDX Health; and receives royalties from Elsevier.