Bold, Innovative Strategies Improve Outcomes for Some of NYU Langone’s Most Critically Ill Patients with COVID-19

Cardiothoracic surgeons at NYU Langone are implementing aggressive strategies to improve the outcomes of patients critically ill with COVID-19.
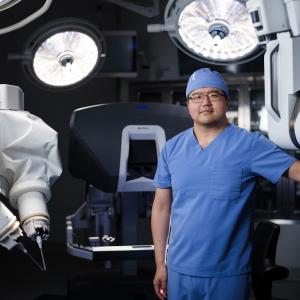
Photo: NYU Langone Staff
As the number of critically ill patients in severe respiratory distress due to 2019 coronavirus disease (COVID-19) who were admitted to NYU Langone Health swelled in late March, it quickly became clear that the medical teams caring for them—largely consisting of critical care specialists and pulmonologists—would need frontline reinforcements to handle the rapid onslaught. Early on, a team from the Department of Cardiothoracic Surgery played a particularly vital role, contributing their highly specialized expertise to this effort.
“For our entire professional career, cardiothoracic surgeons have been caring for patients with major pulmonary injuries and infections, patients who are difficult to wean off ventilators, and patients afflicted by cardiac or pulmonary diseases with multiple causes,” notes Aubrey C. Galloway, MD, the Seymour Cohn Professor of Cardiothoracic Surgery and chair of the Department of Cardiothoracic Surgery. “So bringing our team into this process is like bringing in the Navy Seals, and they have eagerly accepted the challenge.”
Mathew R. Williams, MD, chief of the Division of Adult Cardiac Surgery, who volunteered to care for critically ill patients in the intensive care unit (ICU), was put in charge of the initiative. Dr. Williams, the first physician in the United States to be trained in both cardiothoracic surgery and interventional cardiology, is also director of the Heart Valve Center. “Mat put together a comprehensive plan,” says Dr. Galloway, “and he has done a great job.”
Dr. Williams’s ICU team consists of five cardiothoracic surgeons on the faculty who serve as attending physicians on critical care units at Tisch Hospital and Kimmel Pavilion, as well as three fellows in cardiothoracic surgery who provide care in the ICUs and other areas as needed. Another senior faculty member who volunteered is Nader Moazami, MD, chief of the Division of Heart and Lung Transplantation and Mechanical Circulatory Support, who also serves as an attending in the ICUs. Dr. Moazami, who has performed well over 300 heart transplants, leads the first heart transplant program approved in New York City in more than 15 years. “The teamwork has been incredible,” says Dr. Williams. “The different specialties augment each other. We’re all swept together. This really is a team.”
VIDEO: Dr. Aubrey C. Galloway discusses the strategies being used by NYU Langone’s team of cardiothoracic surgeons to help care for patients in severe respiratory distress due to COVID-19.
Working with colleagues from multiple specialties, other cardiothoracic surgery faculty members have developed and implemented several key clinical strategies that Dr. Galloway says have greatly improved the outcomes of many of the patients most sick from COVID-19. One important contribution was the development of a novel technique for performing a percutaneous tracheostomy, a procedure performed at the beside of patients critically ill with COVID-19, who must remain in isolation. The innovation sprang from Luis F. Angel, MD, an interventional pulmonologist who is medical director of lung transplantation at NYU Langone, and Zachary N. Kon, MD, a cardiothoracic surgeon who is the surgical director of lung transplantation.
With the standard percutaneous tracheostomy, the doctor uses a scope to obtain a clear view of the airway, pulling the endotracheal tube up toward the vocal cords and deflating the device’s balloon, or cuff. But doing so allows infectious aerosolized droplets to escape, endangering the safety of clinicians. Because the procedure is potentially hazardous, most hospitals avoid it for patients with COVID-19, unless it becomes absolutely necessary.
Dr. Angel and his team devised a safer approach. Instead of cutting through the trachea, or windpipe, doctors make a nick in the skin at the base of the neck, insert tubing, and maneuver it between the rings of the trachea. This allows the endotracheal tube to stay in place and the cuff to remain inflated until the ventilator is transferred to the tracheostomy tube, greatly reducing the risk of viral spread. Not only does the procedure subject patients to less sedation and discomfort, but it helps wean them off a ventilator sooner, creating a shorter route to physical therapy and recovery.
Having seen many critically ill patients with similar respiratory issues over the years, Dr. Galloway asked to join his fellow senior attendings on patient rounds in the ICU. He accompanied Robert J. Cerfolio, MD, MBA, chief of clinical thoracic surgery and NYU Langone’s executive vice president and vice dean, chief of hospital operations; Daniel H. Sterman, MD, director of the Division of Pulmonary, Critical Care, and Sleep Medicine; and Mark E. Nunnally, MD, director of adult critical care. “We listened to the intensivists on the front lines,” says Dr. Galloway, “and many of them described the advantages of performing a tracheostomy early on to clear secretions from the airway and wean the patient off sedatives more rapidly.” Nationwide, this approach has been discouraged, but based on the benefits NYU Langone’s senior team observed, early percutaneous tracheostomy has become the institution’s new standard of care for intubated patients with COVID-19.
COVID-19 triggers a severe inflammatory response that fills the lungs with thick, tenacious secretions that often obstruct the airway, leading to oxygen deficiency. To remove these secretions, Michael Zervos, MD, chief of the thoracic surgery service at Tisch Hospital and Kimmel Pavilion, in collaboration with thoracic surgeon Costas Bizekis, MD, formed a team to perform frequent “toilet bronchoscopies” on intubated patients with COVID-19. A bronchoscopy involves inserting a long scope into the lungs to suction out sputum, essentially unclogging them. The procedure, Dr. Zervos explains, prevents segments of the lungs from collapsing, improves oxygenation, and helps prevent bacterial infections.
While bronchoscopy provides immediate and potentially lifesaving relief for patients with COVID-19, the procedure poses a high risk of viral transmission to the doctors who perform it. Nevertheless, Dr. Zervos and his team have accepted the risks because they believe that the benefits for patients are so vital. To lessen the potential for harm, however, they practice a rigorous protocol, which was developed with input from Dr. Cerfolio. So far, none of the physicians who perform bronchoscopies are known to have been infected, and all are tested regularly.
Finally, three of NYU Langone’s transplant surgeons—Dr. Kon, Stephanie H. Chang, MD, a lung transplant and general thoracic surgeon, and Deane E. Smith, MD, a heart transplant and adult cardiac surgeon—have been using a technique called veno-venous extracorporeal membrane oxygenation, or V-V ECMO, to treat patients in respiratory distress who are not responding to a ventilator. The life support system does what the lungs no longer can: remove carbon dioxide from the blood and infuse it with oxygen. The patients who respond best to V-V ECMO are those who are younger and do not have multiorgan failure.
There was little experience to establish the value of ECMO for patients with COVID-19, but Dr. Kon, Dr. Chang, and Dr. Smith thought the technique offered promise. Their instincts paid off. Of the 29 critically ill patients with COVID-19 who were placed on V-V ECMO—all unlikely to survive with standard treatment and mechanical ventilation—more than 40 percent have been weaned from life support, and their lungs have recovered. Most others are progressing well. “This is the largest experience of its kind in the United States, with the best results worldwide,” notes Dr. Galloway. “We have been more aggressive with this approach than most medical centers, and it’s going to save a lot of lives.”
Dr. Galloway says he is deeply gratified by the contributions made by his team, but he attributes the good patient outcomes to NYU Langone’s truly multidisciplinary care. “Considering the great sacrifices that our faculty, nurses, and staff have made to care for patients with this extremely virulent disease,” he says, “it is the least we can do. This is a healthcare crisis, so we have to be all in.”