NYU Langone is 1 of 120 centers that will enroll people in a global phase 2/3 clinical trial testing whether a lead mRNA vaccine prevents COVID-19.
Photo: NYU Langone Staff
The first U.S. patients have been dosed in a phase 2/3 clinical trial testing whether a lead messenger RNA (mRNA) vaccine candidate can prevent infection with the virus that causes 2019 coronavirus disease (COVID-19).
NYU Grossman School of Medicine, under the auspices of NYU Langone Health’s Vaccine Center, served as one of the original sites for the initial stages of the same study that focused on the vaccine’s safety and if it was tolerated well. The next phase—2/3—for which NYU Grossman School of Medicine will also participate as 1 of 120 centers, may enroll up to 30,000 healthy participants aged 18 to 85 globally. The study will measure whether the vaccine candidate can protect against COVID-19 infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Pfizer Inc. and BioNTech SE today announced the trial’s transition into its final stage. Vaccine designers at BioNTech sought to determine which protein components of SARS-CoV-2 were “most noticed by” the human immune system, with the goal of teaching the system to further attack them upon a future encounter with the virus, researchers say.
“It is tremendously encouraging to see the early phase of this trial succeed, and to have a lead candidate emerge for global testing,” says Mark J. Mulligan, MD, director of the Division of Infectious Diseases and Immunology and the Vaccine Center at NYU Langone. “We will continue to engage in rigorous scientific study to learn as soon as possible if this vaccine can be part of the public health solution to this terrible pandemic.”
VIDEO: Infectious diseases expert Dr. Mark J. Mulligan discusses what is entailed in the phase 2/3 clinical trial aiming to test the efficacy of a COVID-19 vaccine candidate.
NYU Langone was chosen as a trial center in part because of Dr. Mulligan’s expertise in infectious disease research programs that have over decades assessed investigational vaccines for HIV and several other viruses including Zika, Ebola, and pandemic influenza.
The study vaccine is part of the class called “mRNA vaccines” that with recent advances can quickly be computer-designed and scaled up into millions of doses if successful and pending regulatory approval using high-speed technologies. RNA-based vaccines also provide a level of safety since it is not possible to catch SARS-CoV-2 virus or COVID-19 disease from the RNA vaccines themselves.
Earlier Trial Phase Successful
mRNA vaccines are based on RNA, or ribonucleic acid, a form of genetic material similar to DNA. Human cells use mRNA to translate DNA instructions into proteins, the workhorse molecules that make up cell structures. In the pandemic coronavirus, RNA serves as the primary genetic material instead of DNA.
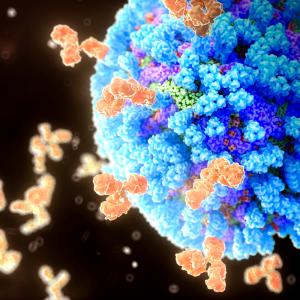
Two of the study vaccine candidates in phase 1 of the trial contained viral RNA encoding the “spike proteins” used by SARS-CoV-2 to attach to proteins on human cell surfaces, the first step in invading the cells in which it multiplies. Including the spikes in vaccines has the potential to make proteins required for viral survival (ability to infect) visible to the human immune system, say the investigators. For this reason, the lead vaccine to move forward into the larger trial, BNT162b2, will encode an optimized SARS-CoV-2 full-length spike glycoprotein, at a 30-µg dose level in a 2-dose regimen.
Such vaccine injections are delivered in small segments of mRNA encoding spike protein into the arm muscles of participants. All vaccine versions are encased in a fatty lipid particle meant to prevent their destruction by enzymes, and to let them persist long enough to enter the cytoplasm of cells in muscle and nearby lymph nodes. Once there, the spike protein is made and triggers the production of antibodies, immune proteins that specifically glom onto this viral target protein, disabling it and tagging it for removal from the body.
The current, ongoing clinical trial began with a phase 1/2A study on May 4, 2020. The company reported today that subjects that received 2 doses of either 10 or 30 µg of BNT162b2 expressing the SARS-CoV-2 spike protein had significantly elevated spike-binding antibodies at day 28 (7 days after dose 2). Also 7 days after dose 2, all subjects who received 10 or 30 µg of BNT162b2 had SARS-CoV-2 “neutralizing antibodies,” capable of defending cells from the virus, and of blocking its biological effects. Local reactions and systemic side effects after immunization were dose-dependent, generally mild to moderate, and short-lived. No serious adverse events were reported by the company.
The phase 2/3 trial is designed as a 1:1 vaccine candidate to placebo, randomized, observer-blinded study to obtain safety, immune response, and efficacy data needed for regulatory review.
If the ongoing studies are successful and the vaccine candidate receives regulatory approval, the companies expect to manufacture up to 100 million doses by the end of 2020 and potentially more than 1.3 billion doses by the end of 2021. On July 22, the U.S. government placed an initial order of 100 million doses for $1.95 billion, with the right to acquire up to 500 million additional doses from the company.
Media Inquiries
Greg Williams
Phone: 212-404-3500
gregory.williams@nyulangone.org