Perlmutter Cancer Center Researchers Build Artificial Intelligence That Teaches Itself How to Spot Gene Mutations
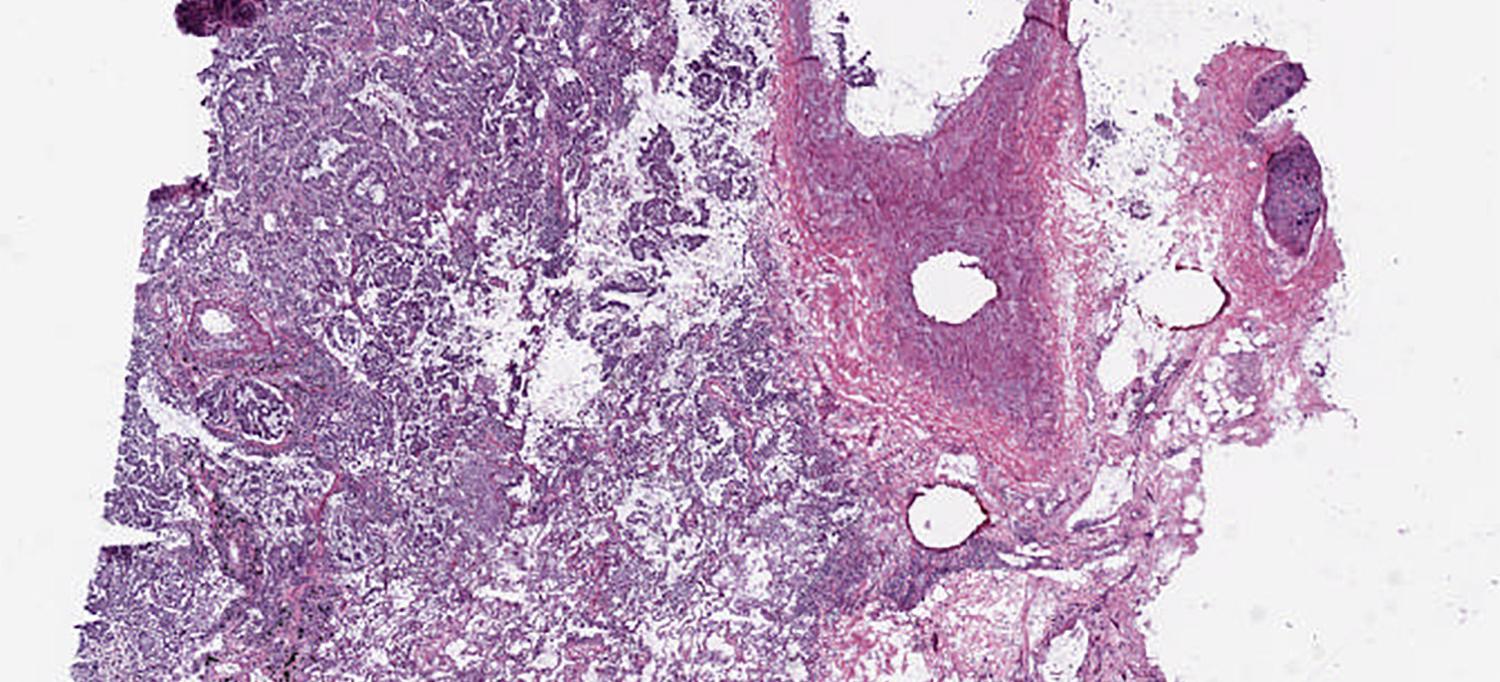
By training on thousands of lung pathology scans like this one, an AI program taught itself how to spot six mutations linked to adenocarcinoma, which could potentially accelerate treatment for eligible patients.
Image: courtesy of Drs. Aristotelis Tsirigos and Narges Razavian
When they decided to collaborate on an artificial intelligence (AI) project to diagnose lung cancer, Aristotelis Tsirigos, PhD, and Narges Razavian, PhD, both understood it was important to let physicians tell them where they needed help from AI, not the other way around. “We needed to hear about the big questions they want answered, and what matters most to patients,” says Dr. Tsirigos, associate professor of pathology at NYU Langone’s Perlmutter Cancer Center.
What they heard back was that patients who get a cancer diagnosis often want reassurance that their clinician has made the right call. “A patient may think their doctor is the best in the world,” he says. “But they know cancer is complex, and they often have some doubts about what they’re hearing from the doctor.” The apprehension is well founded. The National Academy of Medicine estimates that as many as 10 percent of patient deaths can be attributed to misdiagnosis, and false positives can suggest that cancer is present when it isn’t.
The researchers thought that machine learning could provide physicians with another set of eyes, so to speak, to wring correct diagnoses out of images. So they “trained” their AI system by feeding it images to which pathologists had already attached their diagnoses. This allowed the system to determine which sort of visual data in the image, such as texture, color, density, and the distance between cells, tended to be associated with which diagnosis.
Not only could their system distinguish between two of the most common types of lung cancer with 97 percent accuracy, but it was also able to correctly classify 83 percent of the tumors that pathologists had misclassified.
There was also a surprise: the system taught itself to identify six mutations linked to the most common form of lung cancer, adenocarcinoma. That’s something human pathologists could never do from images. Identifying these mutations is critical for determining the best course of treatment for this rapidly metastasizing cancer, but normally it can be done only through DNA sequencing of a biopsy, a costly process that can take weeks.
What’s more, no one really knows how the machine learned this skill. “From our findings, it seems the machine may be flagging subtle changes in a tumor’s appearance,” says Dr. Tsirigos. “But, really, we have no idea how it’s recognizing the mutations.” Right now, the software isn’t always accurate in labeling the mutations, but if the accuracy can be pushed to 90 percent, the researchers plan to seek Food and Drug Administration approval to use the technology clinically and eventually adapt it to other types of cancer, such as melanoma.
Dr. Tsirigos estimates a three-year time frame before some version of the software rolls out in clinical use at NYU Langone and perhaps elsewhere, but he stresses that it will never serve as the sole source of diagnosis. “The goal is to at least help the doctors by providing a quick second opinion,” says Dr. Tsirigos. “We can’t even imagine that the doctor would ever be out of the loop.”

