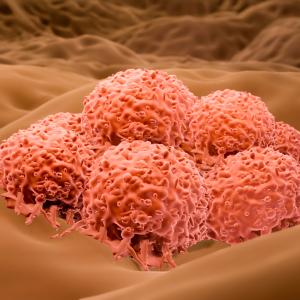
Levels of DNA Fragments Released by Dying Tumor Cells May Serve as an Early Indicator of Treatment Success in Late Stages of One of the Most Aggressive Forms of Skin Cancer

Photo: krisanapong detraphiphat/Getty
A test that monitors blood levels of DNA fragments released by dying tumor cells may serve as an accurate early indicator of treatment success in the late stages of one of the most aggressive forms of skin cancer, a new study finds.
Led by NYU Grossman School of Medicine and Perlmutter Cancer Center researchers, the investigation looked at adults with undetectable levels of freely circulating tumor DNA (ctDNA) four weeks into drug treatment for metastatic melanoma tumors that cannot be removed surgically or are unresectable. The study showed that these patients, all of whom had common genetic changes (BRAFV600 mutations) linked to cancer, were living nearly twice as long without cancer growth as those who continued to have detectable levels.
Normally, the study authors say, physicians would have to wait three months before an X-ray, CT scan, or other measures could reveal whether a tumor is growing or shrinking in response to treatment.
“Our findings suggest that levels of ctDNA may serve as a fast and reliable tool to gauge whether an anticancer medication is working,” says study senior author David Polsky, MD, PhD. “The blood test results could help support continuing the current treatment strategy or else encourage patients and physicians to consider other options,” adds Dr. Polsky, the Alfred W. Kopf, MD, Professor of Dermatologic Oncology at NYU Langone Health and member of Perlmutter Cancer Center.
Dr. Polsky notes that swift treatment modification could potentially be helpful in a disease as aggressive as melanoma, which kills nearly 7,000 Americans a year and is notoriously difficult to treat once it spreads to other body parts. Early feedback from a blood test might save lives, he says.
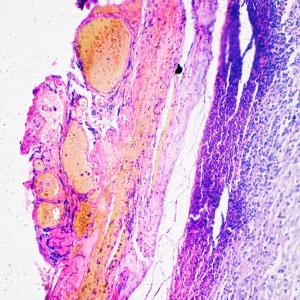
Researchers have long searched for better ways to monitor certain cancers using blood tests, or so-called biomarkers, which can be performed more easily, more often, and less expensively than imaging scans or surgical procedures and provide a clearer picture of tumor behavior over time. With melanoma, one frequently used option, a test for the presence in blood of an enzyme called lactate dehydrogenase (LDH), has had only limited success as such a tool, because non-cancer ailments such as liver injury and bone damage can also cause levels to spike. Although more specific biomarkers have been identified in cancers of the prostate, breast, and colon, the study investigators say a reliable signpost for melanoma has until now remained elusive.
According to Dr. Polsky, also a professor in the Department of Pathology at NYU Langone, early research by the same team had pointed to ctDNA as a promising candidate. This method works by targeting the most common mutations in the DNA code found in melanoma cells. This mutated DNA spills into surrounding blood as the cancer cells break down. In previous small studies, the blood test was shown to outperform LDH in predicting melanoma recurrence, as well as tracking progression of other forms of cancer.
The new investigation, published online February 12 in the journal The Lancet Oncology, was conducted over two years and is the largest analysis to date of the potential utility of this blood test for skin cancer, says Dr. Polsky.
For the study, the research team analyzed blood samples from 2 pivotal clinical trials involving 383 American, European, and Australian men and women. All were receiving targeted treatment with drugs dabrafenib and trametinib for unresectable metastatic melanoma tumors that had mutations in the BRAF gene, which is found in about half of all patients with the disease, investigators say. The investigators measured levels of ctDNA from patients whose tumors had this mutation before treatment and one month into therapy. As part of the clinical trial, patients received periodic checkups using CT scans until treatment ended.
Among the study’s other findings were that patients with 64 or fewer copies of ctDNA per milliliter of blood before treatment were likely to respond well to therapy, surviving nearly 3 years on average. By contrast, levels above that threshold were linked to a significantly poorer chance of survival, with patients living just over a year.
The investigators say the blood test is highly reliable, as they were able to detect ctDNA in 93 percent of patients. These blood test results were also reproduced in a second group of patients in the same stage of the disease who were enrolled in another clinical trial.
“Although this gene-based test focuses on tumors with BRAFV600 mutations, we believe it will be similarly useful for melanomas that have other mutations, such as defects in the NRAS and TERT genes, which are also commonly mutated in this disease,” says study lead author Mahrukh Syeda, MS. “Ultimately, we’d like to see this test used routinely in the clinic to help guide treatment decisions,” adds Syeda, a research scientist in the Ronald O. Perelman Department of Dermatology at NYU Langone Health.
She cautions that the blood test is not yet U.S. Food and Drug Administration (FDA) approved, but notes that the evidence of its accuracy and value supports future applications for approval to make it available for clinical use.
Syeda says the team next plans to evaluate the ctDNA approach in patients who have earlier stages of melanoma.
Funding support for the study was provided by Novartis Pharmaceuticals Corporation in East Hanover, New Jersey.
Besides Dr. Polsky and Syeda, other NYU Langone researchers are Jennifer Wiggins, PhD; and Broderick C. Corless, BS. Other co-investigators are Georgina Long, MD, at the University of Sydney; Keith Flaherty, MD, at Harvard Medical School in Boston; Dirk Schadendorf, MD, at the German Cancer Consortium in Heidelberg; Paul Nathan, MD, at East and North NHS Trust in Northwood, England; Caroline Robert, MD, at Paris-Sud University in Villejuif, France; Antoni Ribas, MD, at the University of California in Los Angeles; Michael Davies, MD, at the University of Texas in Houston; and Jean Jacques Grob, MD, at Aix-Marseille University in France. Additional authors were Eduard Gasal, MD, and Mahtab Marker, PhD, at Novartis; Matthew Squires, PhD, at Novartis Institute for BioMedical Research in Cambridge, Massachusetts; and James Garrett, PhD, and Jan Brase, PhD, at Novartis Pharma AG in Basel, Switzerland.
Media Inquiries
Shira Polan
Phone: 212-404-4279
shira.polan@nyulangone.org