An experimental compound prevents the virus that causes 2019 coronavirus disease (COVID-19) from entering human airway cells, a new study finds.
Posted online recently on the preprint server bioRxiv, the work revolves around the structure of SARS-CoV-2, the virus causing the current pandemic. This virus has on its surface a spike protein that can attach to angiotensin converting enzyme 2 (ACE2), a protein on the surface of cells lining human lungs. Once attached, the spike pulls the virus close to a cell, which lets it fuse to it and enter it, and then hijack the cell’s machinery to make copies of itself, researchers say.
For this reason, molecular biologists have sought to engineer forms of ACE2 that, instead of being woven onto the cell surface, float freely. They hoped that free-floating ACE2 could serve as a decoy that competes with the membrane-bound counterpart for the viral spike protein, thereby blocking virus entry.
Led by researchers at NYU Grossman School of Medicine, a new investigative effort made key changes to a free ACE2 molecule, and then fused one part of it to a piece of an antibody, an immune system protein, with the goal of strengthening its antiviral effect. The team calls their molecule an “ACE-2 microbody.”
“In our tests, the ACE-2 microbody was about 10 times as effective at blocking virus entry as unmodified forms of ACE2 studied previously,” says corresponding study author Nathaniel R. Landau, PhD, professor in the Department of Microbiology at NYU Langone Health. “We call our compound a microbody because, by using just the key parts of each protein, the drug molecule is smaller and potentially easier to make than versions made up of complete proteins.”
The researchers caution that any signals of effectiveness for the experimental drug would need to be confirmed in animal studies, and then in human trials if appropriate.
Building on HIV Experience
To build the microbody, the study authors used a standard technique in molecular biology, which creates a “fusion protein” by building a DNA molecule in which two genes, each with instructions for a different protein, are linked. The linked genes are then introduced into a mammalian cell, which makes the hybrid protein from the hybrid instructions.
For the current work, the researchers started with the ectodomain of ACE2, the part of the protein that sticks out from a cell’s surface and attaches to the viral spike protein. They changed the ectodomain’s genetic code to swap out one amino acid building block, replacing a histidine at position 345 in the protein’s structure with an alanine. The modification kept ACE-2 from interacting with angiotensin, a hormone that regulates blood pressure, its natural role and a possible source of side effects.
For the second piece of their fusion compound, the study authors used an Fc domain, the part of an antibody’s structure that turns on other parts of the immune system when the antibody encounters an invading microbe. The team intentionally shortened the domain, however, to prevent off-target immune effects.
The team wanted the Fc domain on the microbody because such proteins form strong disulfide bonds when they encounter one other. The binding of two fusion proteins through their Fc domains creates a dimer, a stable structure that attaches more strongly to the virus because it now has two ACE2 ectodomains to cling to viral spikes, researchers say.
To determine how strongly their experimental drug could interact with the COVID-19 virus, the research team used a “pseudotyped” virus, a vital tool used in decades of HIV research. To make it, the authors started with HIV viruses, but removed the disease-causing part of their genetic material to make them safe to work with.
To these engineered viral particles the team then added the SARS-CoV-2 spike protein, as well as a gene encoding the firefly protein luciferase.
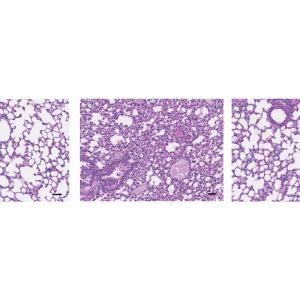
Like the current coronavirus, the pseudotyped virus could infect cells by using the SARS-CoV-2 spike to attach to ACE-2. With the firefly gene included, cells infected by the test virus glowed, and glowed brighter the more viral particles they were infected with. By mixing the ACE-2 microbody with the pseudotyped virus, infecting cells, and then measuring the glow, the researchers could tell how well their new molecule blocked viral entry.
“An advantage of the study drug is that, by competing for the spike with the ACE2 membrane–bound receptor, infection is blocked before it can start,” says first study author Takuya Tada, PhD, a postdoctoral scholar in Dr. Landau’s lab. “Coronaviruses are quick to evolve around treatments, like therapeutic antibodies, that target one structural feature on the virus, but will have a harder time changing the entire first step by which they enter cells.”
Along with Dr. Landau and Dr. Tada, other study authors from NYU Grossman School of Medicine were Kenneth Stapleford and Ramanjit Kaur. Also study authors were Chen Fan and Crina Nimigean in the Department of Anesthesiology at Weill Cornell Medical College, as well as Harry Gristick in the Division of Biology and Biological Engineering at California Institute of Technology. The work was funded by National Institutes of Health grants DA046100, AI122390, AI120898, and P01-AI38398-S1. The study has been submitted to a peer-reviewed journal, and is under consideration for publication.
Media Inquiries
Greg Williams
Phone: 212-404-3500
gregory.williams@nyulangone.org