Medical & Cosmetic Outcomes Weighed for Patient with Neurofibromatosis Type 1

Dr. Donato R. Pacione and Dr. Seth M. Lieberman planned a complex endoscopic approach to safely reach and fully resect a patient’s orbital tumor.
Photo: NYU Langone Staff
A patient previously treated at NYU Langone Health for a left orbital tumor returned for treatment of a secondary tumor whose rapid growth—and associated eye proptosis—indicated a second resection. Balancing desired medical outcomes with the cosmetic concerns of a traditional invasive approach, a multidisciplinary team combined surgical expertise, planning a complex endoscopic approach to safely reach and fully resect the tumor.
Persistent Tumor Demands Intervention
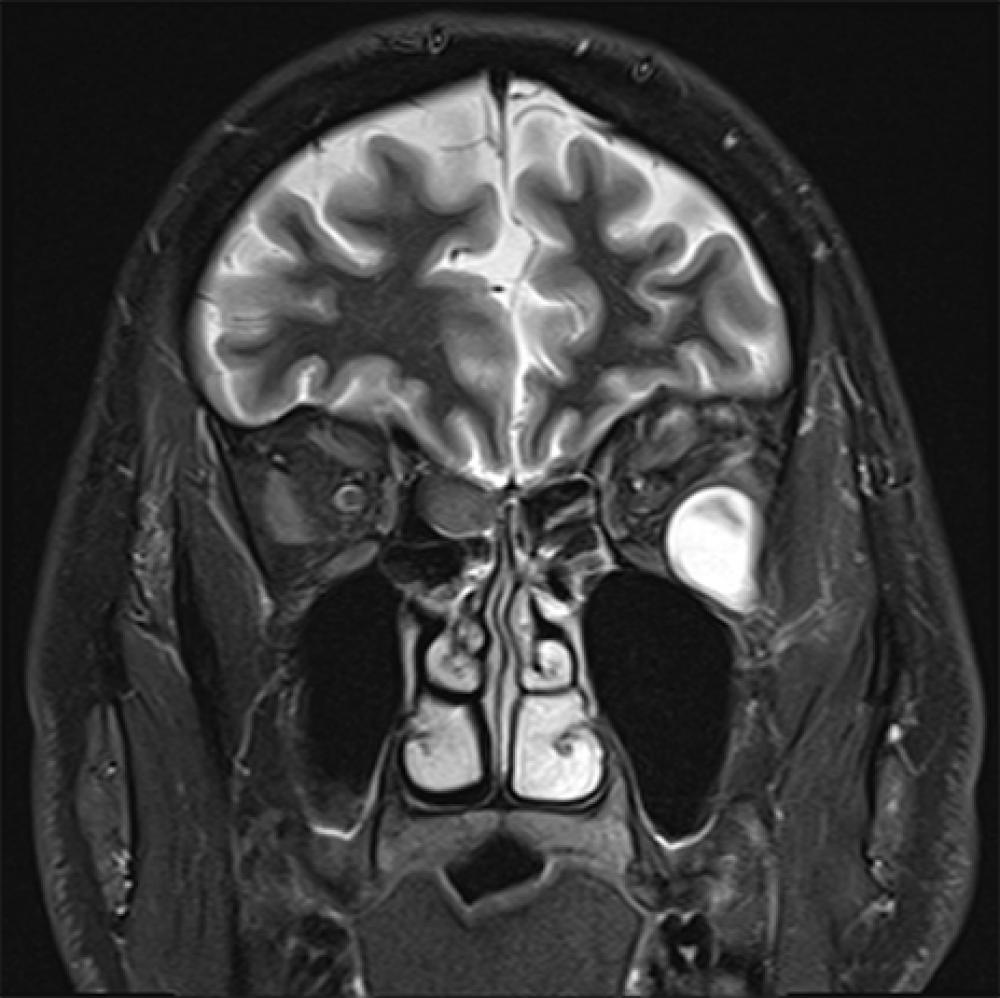
The patient had initially presented two years prior for a consultation with Donato R. Pacione, MD, assistant professor in the Department of Neurosurgery, for progressive eye proptosis with associated pressure and pain. An MRI demonstrated the presence of two peripheral nerve sheath tumors of the left orbit (one superior and one inferolateral), and mosaic neurofibromatosis type 1 (NF1) was suspected. At that time, Dr. Pacione recommended resecting the larger, superior tumor transorbitally, with a minimally invasive approach through the eyelid.
Because the secondary tumor was significantly smaller and asymptomatic, and removing it was considered overly aggressive in a single surgical setting, watchful waiting was recommended. “That second tumor sat underneath the eye and at that time was not causing symptoms,” notes Dr. Pacione. “Resecting it along with the first tumor could have put undue pressure on the eye, but we knew it could eventually compromise vision and require removal.”
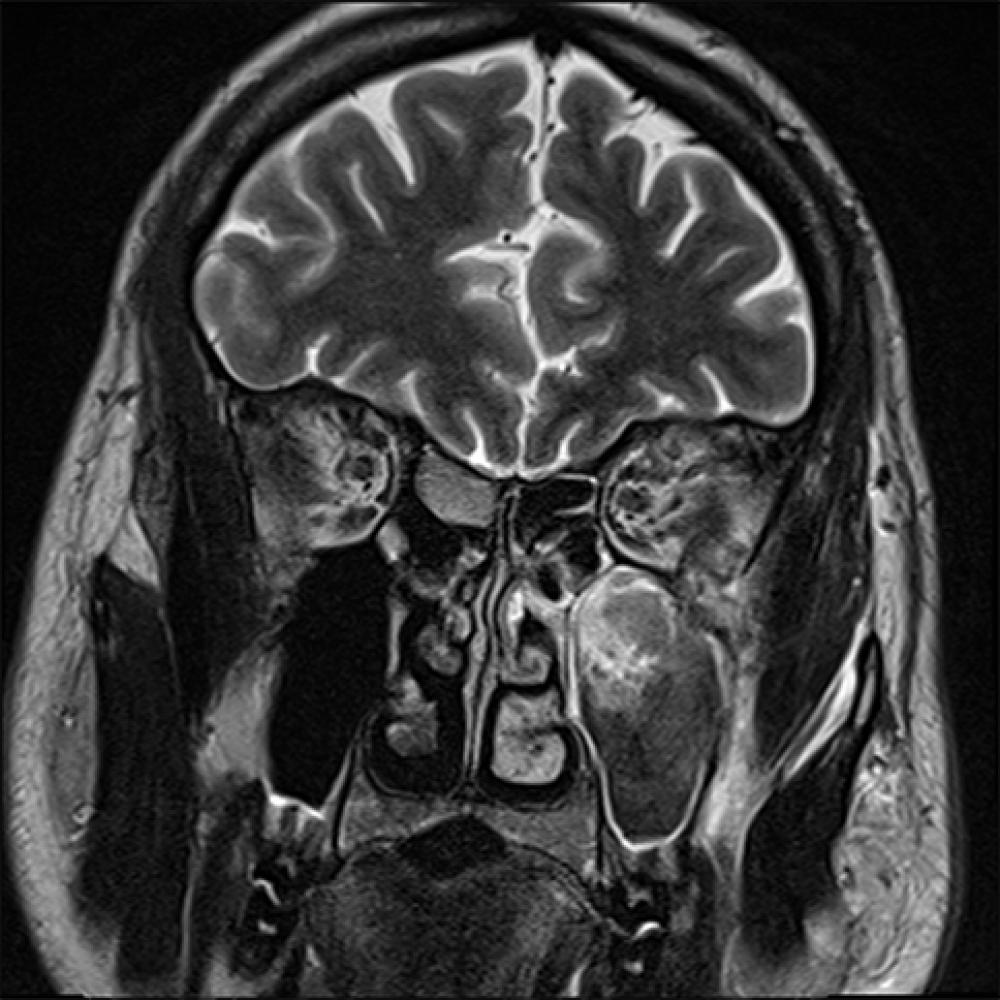
Eighteen months later, the patient returned with recurring eye proptosis, and new imaging confirmed progressive growth of the secondary tumor, which was now about 2 cm in diameter. Although surgical intervention was now a necessity in order to prevent further symptom development, the tumor’s location along the inferolateral orbit added another layer of complexity.
Such a challenging tumor location generally necessitates an open surgical approach with an osteotomy to gain access, with cosmetic implications that troubled the patient. The combination of complexities prompted a consultation with Seth M. Lieberman, MD, assistant professor in the Department of Otolaryngology—Head and Neck Surgery, whose endoscopic surgical expertise was critical to identifying the optimal approach.
Cosmetic Concerns Inform Alternative Approach
Typically, a tumor of this magnitude would necessitate a full orbitotomy—which involves removing the lateral wall of the orbit through the eyelid and cutting and removing the bone on either side of the orbit, which then requires reconstruction once the tumor is resected. For this patient, the cosmetic disfigurement that can result from such an approach was untenable.
However, this tumor’s location, between the inferior rectus and the lateral rectus, made it more amenable to an endoscopic-assisted approach. Dr. Lieberman and Dr. Pacione deliberated over the options, and then together crafted a careful surgical plan relying on strategic endoscopic “ports” to safely reach the tumor.
“The location of this tumor, deep in the periorbita, made reaching it particularly challenging,” notes Dr. Lieberman. “You’re trying to get good visualization of and surgical access to the lesion using straight instruments in a small space, and it involves a high degree of difficulty that demands experience.”
Risks of such an approach include injury to the muscles and nerves within the orbit, as well as injury to the nasolacrimal duct. Additionally, the patient was advised that due to the tumor’s location adjacent to the infraorbital nerve, surgery would likely result in loss of facial sensation. However, in light of the tumor’s growth and the patient’s desire for both function preservation and a good cosmetic outcome, the decision was made to proceed endoscopically.
Dr. Lieberman used both a sublabial approach, by making an incision under the lip, and a transnasal prelacrimal approach. “The tumor was way out toward the lateral part of the orbit, adding to the difficulty of reaching it, since most endoscopic approaches to the orbit are more medial,” notes Dr. Lieberman. “So this lateral access was important.”
Though the difficulty of resecting such a tumor is unknown until surgery begins, adds Dr. Lieberman, the approach itself often constitutes the most time-intensive portion of the surgery. Once this patient’s tumor was reached, it was observed to have excellent access and exposure with a clean plane and few adhesions, though it was intimately associated with the infraorbital nerve. The tumor was safely resected in an en bloc fashion, and the tumor cavity was observed to be free of tumor bulk with clear visualization to the inferior rectus muscle as well as the lateral rectus muscle. Dr. Lieberman performed the closure, and the patient was sent to recovery.
Shared Outcomes Reached with Multidisciplinary Planning
With a complex, carefully planned, minimally invasive approach, Dr. Lieberman was able to resect the tumor while leaving the patient cosmetically intact without the need for orbital reconstruction. Although the patient did experience the expected facial sensation loss, he is doing well, and other early NF1-associated tumors appear stable.
“By considering the approach in a stepwise fashion with a multidisciplinary team, we were able to carefully consider the risks and benefits of each method and create positive medical and cosmetic outcomes for this patient,” adds Dr. Lieberman.