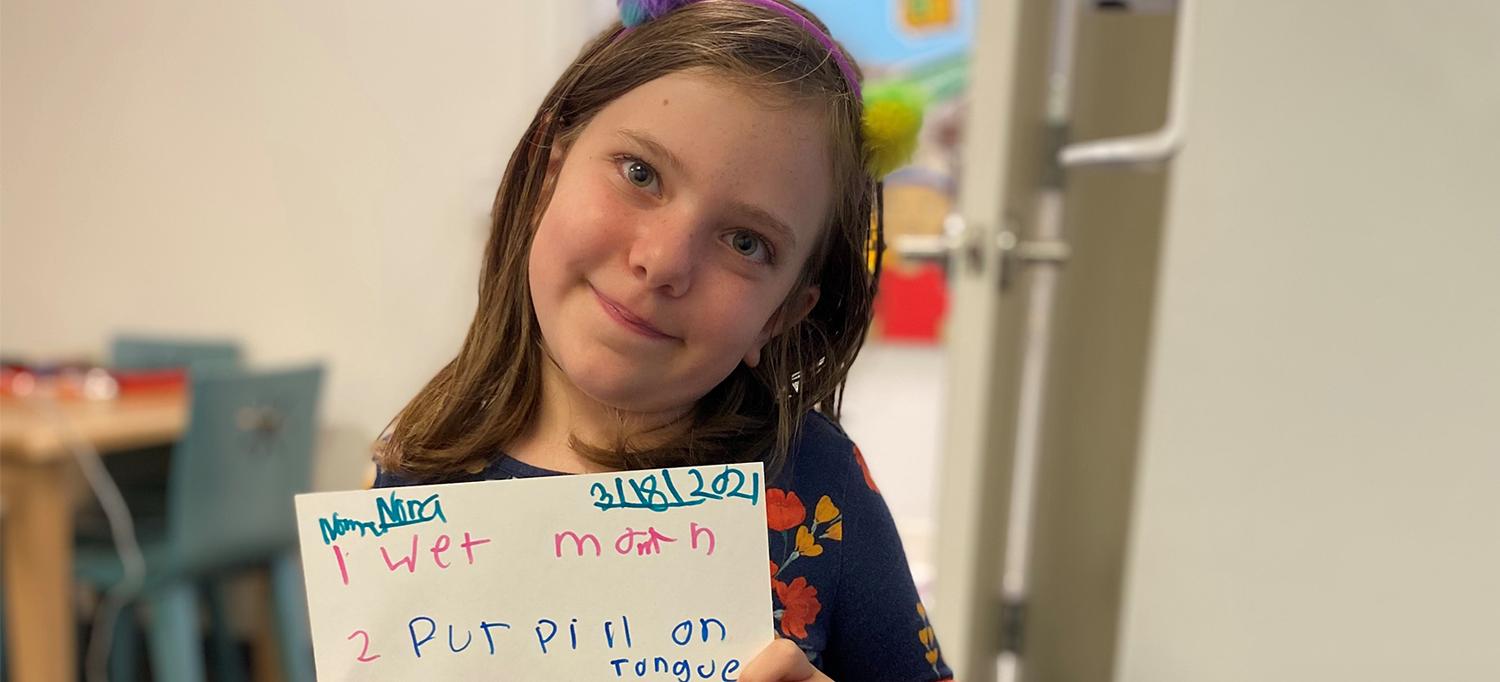
Nora Osterman-Davis has been taking part in a neurofibromatosis clinical trial at the Stephen D. Hassenfeld Children’s Center for Cancer and Blood Disorders, for which she had to learn how to take pills.
PHOTO: HEATHER OSTERMAN-DAVIS
Just in time for Christmas, 8-year-old Nora Osterman-Davis, a patient with neurofibromatosis type 1 (NF1), learned that her brain tumor is now 50 percent smaller, thanks to a clinical trial at the Stephen D. Hassenfeld Children’s Center for Cancer and Blood Disorders, part of Hassenfeld Children’s Hospital at NYU Langone.
Nora has a genetic condition called NF1 that causes benign tumors to grow on nerve tissue inside a person’s brain and in the peripheral nervous tissue. NF1 is the most common type of neurofibromatosis, affecting about 1 in 3,000 people around the world, according to the Children’s Tumor Foundation.
The first symptom appeared at the end of July 2021, when family noticed that Nora needed to hold pages of her books very close to her face in order to read them. A subsequent MRI obtained in August revealed large optic pathway brain tumors, those found along the visual system, that were causing vision loss and frequent headaches for Nora.
“Even though the tumor is non-cancerous, it’s not really ‘benign’ because of its large impact on Nora’s life,” says Robyn M. Borsuk, MD, clinical assistant professor in the Department of Pediatrics and part of Nora’s care team.
Upon diagnosis at NYU Langone’s Comprehensive Neurofibromatosis Center, Nora and her family met with Theodore P. Nicolaides, MD, the Otto and Marguerite Manley and Making Headway Foundation Associate Professor of Pediatric Neuro-Oncology in the Department of Pediatrics and director of the Section of Pediatric Neuro-Oncology at the Stephen D. Hassenfeld Children’s Center for Cancer and Blood Disorders, to determine the best form of treatment. Nora qualified for a randomized phase 3 clinical trial for an MEK inhibitor called selumetinib on August 31, 2021.
Since 2012, NYU Langone has been among 15 medical centers nationwide (and the only site in the tristate area) conducting clinical trials of experimental therapies for neurofibromatosis. Some of the medications, approved for treating cancer, inhibit the cellular pathway that promotes tumor growth by targeting the enzyme called MEK (or mitogen-activated protein kinase kinase). Nora’s treatment requires her to take 6 pills per day for 24 months and can be better tolerated than traditional chemotherapy.
After just 3 months, Nora’s latest MRI scan revealed that the benign tumor growing on the optic pathway inside her brain had shrunk to be about 50 percent smaller since the initial scan. “Getting a tumor to shrink is one thing—that’s good—but also most importantly, for her the tumor has a functional consequence, meaning it had affected her vision,” says Dr. Nicolaides. “So, this has improved her vision significantly. That’s the most important thing here.”
Nora has some words of wisdom for other kids with NF1 or a brain tumor: “It can be a bit hard and stressful at first, but as you keep doing it, you can get used to it. And you can have a lot of people on your side that know what it’s like to have a brain tumor.”
Read more from SurvivorNet.

