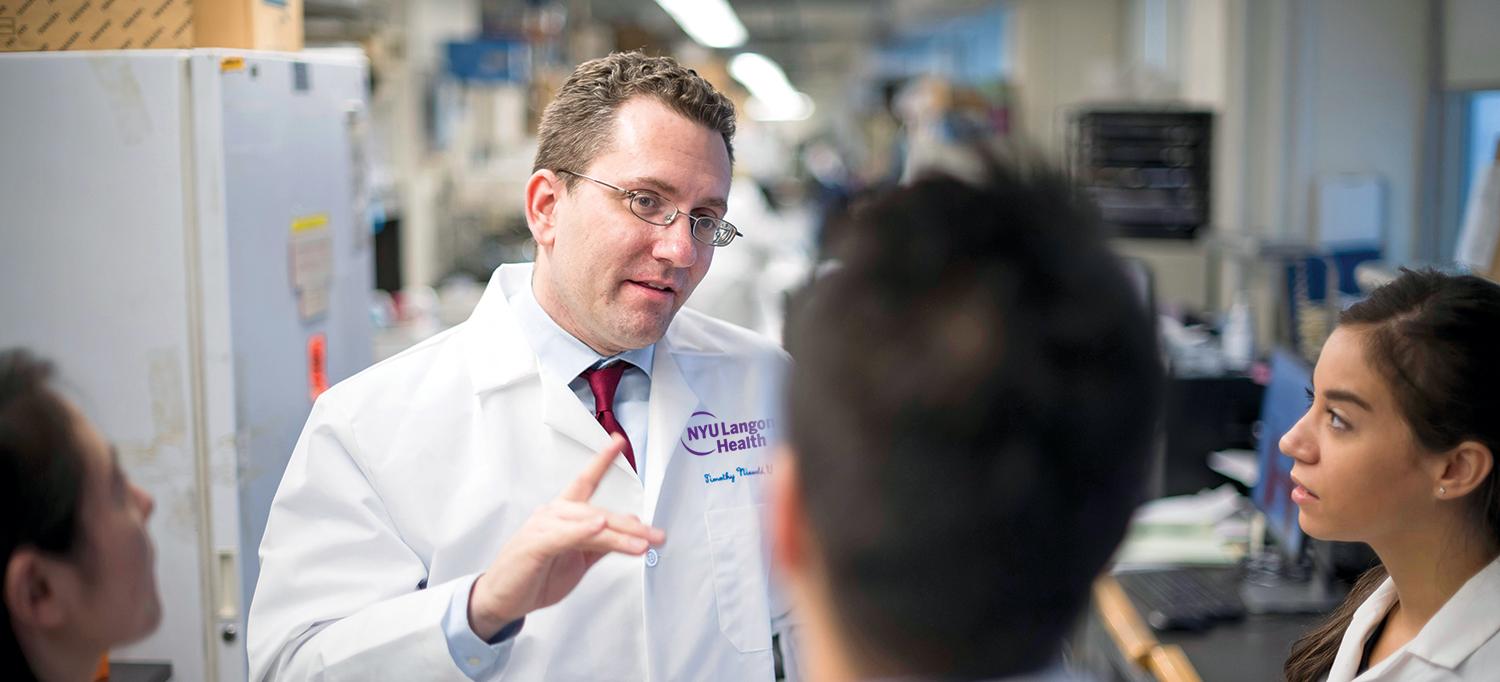
Dr. Timothy B. Niewold
PHOTO: KARSTEN MORAN
With a new director, new faculty, and a half-dozen internally funded pilot projects, the Judith and Stewart Colton Center for Autoimmunity is connecting a diverse group of researchers and aiding a promising range of collaborative efforts at NYU Langone Health.
Timothy B. Niewold, MD, the recently recruited director of the Colton Center, says the three-year-old center is unique in its mission: engaging in cross-disciplinary autoimmune disease research that bridges rheumatology, immunology, genetics, structural biology, neuroimmunology, and other medical specialties.
The Colton Center has made new strides toward that goal with an internal pilot project to foster collaborations and support for “outside the box” ideas, says Dr. Niewold, who arrived in 2017 from the Mayo Clinic. Providing seed money to many diverse ideas, he notes, increases the odds of a breakthrough.
“If you’re funding a large group of people, there will likely be natural synergies and ways that research can come together, even if it’s not apparent when they start,” he says.
Uncovering the Genetic Roots of Autoimmune Disease
Dr. Niewold’s lab has embarked on its own grant–funded pilot project with Jef D. Boeke, PhD, professor of biochemistry and molecular pharmacology and director of the Institute for Systems Genetics. Dr. Boeke’s new method for creating artificial chromosomes, a system he calls the Genome Foundry, enables researchers to partially or completely rewrite chromosomes and recombine them into cell lines.
Dr. Boeke’s method may allow researchers to more easily express variants of still mysterious autoimmune disease risk genes in relevant cell lines to better understand which gene portions may drive the disease-associated dysfunction.
“That brings us closer to understanding this big question: How do the genes cause disease?” says Dr. Niewold.
In particular, the research may enable a more direct examination of human pathogenesis by allowing researchers to use human cell lines and work with the genome in its native structure, targeting specific genetic changes and observing the result.
A Growing Body of Research
Dr. Niewold points to several other center pilot projects that could likewise deliver big dividends. One project, led by Boris Reizis, PhD, professor of medicine and pathology, and Timothy J. Cardozo, MD, PhD, associate professor of biochemistry and molecular pharmacology, is geared toward making a stable form of the enzyme DNase IL3, which is being studied at NYU Langone’s Translational Center of Molecular Profiling and Preclinical and Established Lupus, COMPEL, program.
If successful, the project could lead toward a new type of treatment: DNase replacement therapy for deficient individuals and for patients with lupus who are found to have a dysfunction of this enzyme.
Separate investigations into auto-immune diseases’ genetic and biological mechanisms include a related study by postdoctoral fellow Taro Iwamoto, PhD, a member of Dr. Niewold’s research team; an investigation using blood samples to personalize treatments for rheumatoid arthritis patients by Theresa L. Wampler Muskardin, MD, assistant professor of medicine; research into the interferon- producing cells involved in lupus by cellular immunologist Mark Jensen, PhD assistant professor of medicine; investigations into the genetic basis of lupus by bioinformatics expert Yogita Ghodke-Puranik, PhD assistant professor of medicine; and mouse models of kidney disease created by Amrutesh S. Puranik, PhD, to support the lab’s investigations of lupus nephritis.
A Connective Center of Knowledge
By hosting regular meetings and seminars where researchers can share their best ideas about autoimmune disease, Dr. Niewold notes, the Colton Center is becoming an important gathering and networking place for the scientific community. The center’s design means that gastroenterologists studying inflammatory bowel disease and neurologists looking into multiple sclerosis can learn from each other in ways that inform and aid both efforts.
“In essence, the Colton Center will become the link that helps connect the dots between autoimmune disease mechanisms,” Dr. Niewold adds.