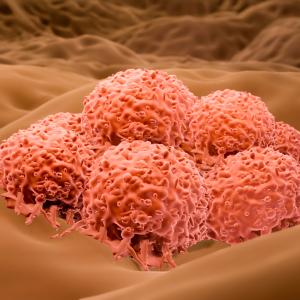
PHOTO: TEK IMAGE/SCIENCE PHOTO LIBRARY/Getty
Blood tests that track the amount of tumor DNA can—after only one month of drug therapy—detect how well treatment is working in patients with skin cancer, a new study finds.
Led by researchers from NYU School of Medicine and Perlmutter Cancer Center, the study takes advantage of the nature of cancer cells, which die and are replaced by new cells continuously as part of aggressive cancer growth. Tumor cells burst as they die, spilling their DNA into the bloodstream, where it can be measured by tests, enabling improved diagnosis and better targeting of treatment based on each individual tumor’s DNA.
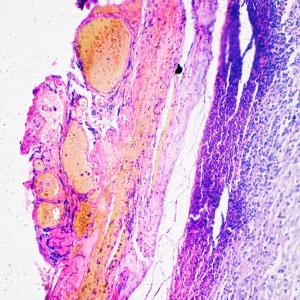
For the new study, researchers traced circulating tumor DNA, or ctDNA, for the cancer gene BRAF, a gene that plays a key role in many types of melanoma, the most aggressive form of skin cancer. In the United States, more than 7,200 individuals are expected to die from metastatic melanoma in 2019, with BRAF mutations playing a role in nearly half of such diagnoses, according to The Skin Cancer Foundation.
“Our study offers firm evidence that tracking this genetic information may be helpful in identifying patients whose cancers shrink and who survive longer as a result of a particular drug regimen,” says senior study investigator David Polsky, MD, PhD, the Alfred W. Kopf, MD, Professor of Dermatologic Oncology and the Department of Pathology at NYU Langone Health.
For the study, being presented at the 2019 American Society of Clinical Oncology annual meeting on June 1 in Chicago, researchers analyzed blood samples from 345 male and female patients with stage III or IV melanoma, which had already spread from the skin to other organs, and who had BRAF mutations.
These patients could not be treated surgically and were part of a larger group of patients participating in a clinical trial of the drugs dabrafenib and trametinib, designed to target BRAF-mutated cancers.
Among the study’s key findings was that the tumor’s BRAF mutation could be detected by the new blood test in 93 percent of the patients before treatment started. In addition, the research team found that BRAF ctDNA levels were no longer detectable after one month of therapy in the 40 percent of patients who had a positive clinical outcome after targeted therapy (as measured by an average survival time of 28 months). By contrast, the 60 percent of patients who did not respond as well still had detectable ctDNA levels, and survived for an average of just 14 months.
Dr. Polsky and his colleagues say this test appears to be more revealing than the current standard test, which measures lactate dehydrogenase (LDH), an enzyme often elevated by melanoma, because fluctuations in LDH often do not accurately predict treatment success or failure.
The typical method of identifying disease progression for these melanoma patients is through CT scans every three months. But Dr. Polsky says the blood test in the current study, noted as the largest BRAF detection rate in patients’ blood to date, suggests it may be helpful to doctors because these tests can be done more frequently and efficiently, and results could be available within a few days.
“If further testing proves successful, monitoring blood samples for BRAF could give us an early indication of whether or not we need to adjust a patient’s treatment plan,” says Dr. Polsky, dermatologist and director of the pigmented lesion service at NYU Langone.
Researchers next plan to test the efficacy of monitoring patient blood samples over longer periods of time, such as several months. They also hope to open a clinical trial to determine whether treatment decisions based on these test results improve patient survival.
Novartis Pharmaceuticals of East Hanover, New Jersey, funded the clinical trial of their drugs, and provided the blood samples and clinical data used in the study, which they also funded. The ctDNA test was developed by Bio-Rad Laboratories in Hercules, California.
Besides Dr. Polsky, other NYU Langone researchers include Mahrukh M. Syeda, MS; Jennifer M. Wiggins, PhD; and Broderick Corless, BS. Additional investigators include Georgina V. Long, MD, PhD, at Melanoma Institute Australia, The University of Sydney, and Royal North Shore and Mater Hospitals in Australia; Keith Flaherty, MD, at Dana-Farber Cancer Institute in Massachusetts; Dirk Schadendorf, MD, at Essen University Hospital and the German Cancer Consortium in Germany; Paul D. Nathan, MD, at Mount Vernon Cancer Centre in the United Kingdom; Caroline Robert, MD, PhD, at Institut Gustave Roussy and Paris-Sud University in France; Antoni Ribas, MD, PhD, at University of California, Los Angeles; Michael A. Davies, MD, PhD, at MD Anderson Cancer Center in Texas; Jean-Jacques Grob, MD, PhD, at AIX-Marseille University in France; and Eduard Gasal, Matthew Squires, Mahtab Marker, and Jan C. Brase at Novartis based in Switzerland.
Media Inquiries
Jamie Liptack
Phone: 212-404-4279
jamie.liptack@nyulangone.org