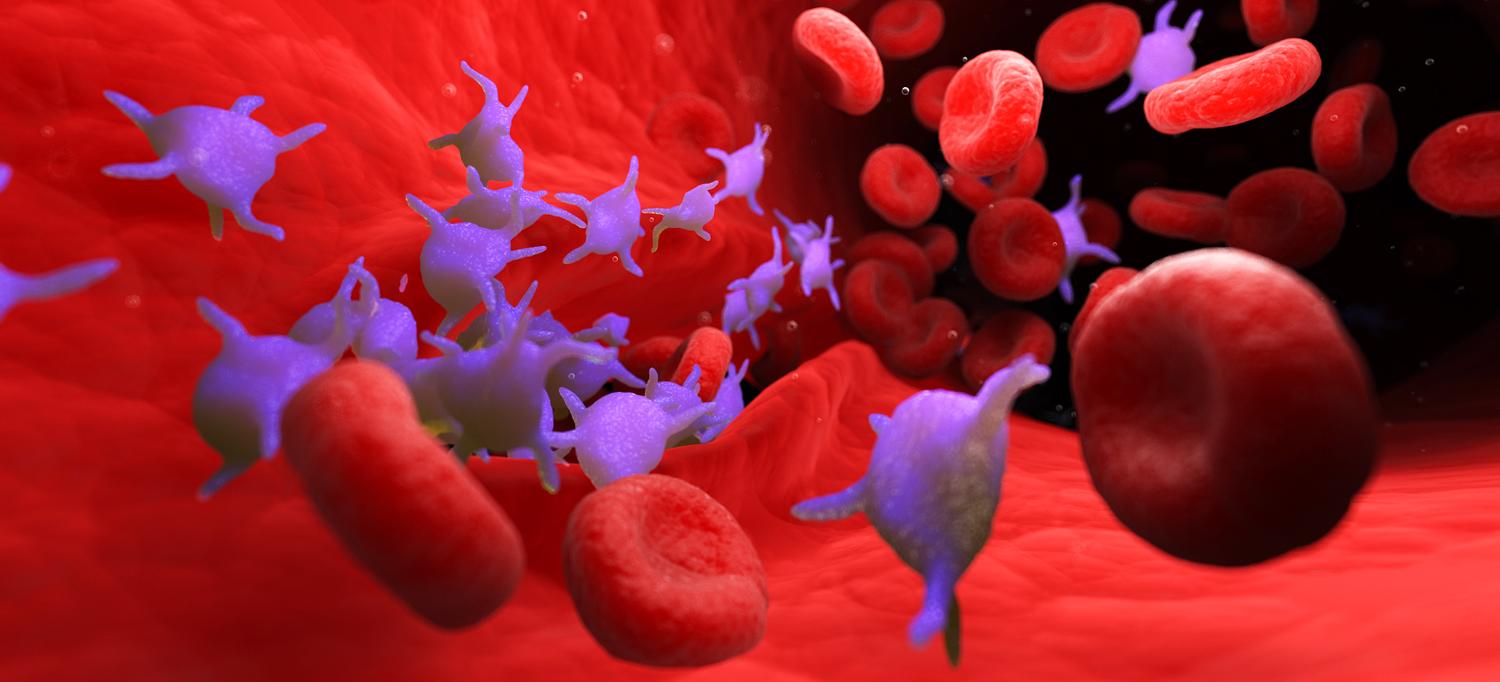
Credit: Getty/SEBASTIAN KAULITZKI/SCIENCE PHOTO LIBRARY
Platelets are circulating cell fragments known to clump up and form blood clots that stop bleeding in injured vessels. Cardiologists have long known that platelets can become “hyperreactive,” causing abnormal clotting that blocks arteries and contributes to heart attack, stroke, and poor blood flow (peripheral artery disease) in the legs of millions of Americans.
Despite this contribution to cardiovascular risk, routine measurement of whether each patient’s platelets clump (aggregate) too much has been infeasible. This is because results delivered by the method typically used to determine platelet activity, called platelet aggregometry, vary too much from lab to lab.
To address this challenge, a new study, led by researchers at NYU Grossman School of Medicine, precisely identified a group of patients with platelet hyperreactivity, and then surveyed them to reveal 451 genes whose activity differed significantly in those with hyperreactive platelets versus those without.
Published online August 20 in Nature Communications, the research team then used bioinformatics to assign a weight to each genetic difference and generate each patient’s Platelet Reactivity ExpresSion Score (PRESS).
“Our results demonstrate that our new plateletcentric scoring system can, for the first time and across populations, circumvent aggregometry to reliably predict platelet hyperreactivity and the related risk of cardiovascular events,” said corresponding study author Jeffrey S. Berger, MD, director of the Center for the Prevention of Cardiovascular Disease at NYU Langone.
The researchers found that their new score can detect platelet hyperreactivity, both in patients at imminent risk of heart attack and in healthy patients whose future risk may otherwise remain unknown.
“Physicians currently prescribe aspirin, a medication that counters platelet activity, to patients based on available risk factors, including high cholesterol or high blood pressure, which are not directly related to platelet function,” added Dr. Berger. “PRESS promises to help physicians confine antiplatelet treatment to the people most likely to benefit: those with platelet hyperreactivity.”
By acting on platelets, aspirin is known to protect against abnormal clotting, but in doing so, increases risk of bleeding, said the study authors. The field needs a reliable way to identify patients for whom protection against heart attack outweighs bleeding risk.
Platelet Score
Progress toward the design of the PRESS began with a shift in the field away from aggregometry methods, which expose platelets to high doses of proteins known to strongly encourage aggregation. Platelets that do not aggregate under these extreme conditions are labeled dysfunctional, but these tests were not designed to directly assess hyperreactivity.
Experience on Dr. Berger’s team and in other labs working with platelets led to a switch to an aggregometry method that instead exposes platelets to a very small dose (4 micromoles, μM) of epinephrine known to weakly encourage aggregation. The field settled on 60 percent aggregation in platelet sample at 0.4 μM of epinephrine as the threshold over which platelets would be designated as hyperreactive. Although this method is not new, the current study provided new evidence that patients meeting this hyperreactivity definition are at much greater risk for cardiovascular events.
Specifically, the team used the newer but still labor-intensive aggregometry method to track the impact of platelet activity status on MACLE (major adverse cardiovascular and limb events), a composite measure of death, heart attack, stroke, and lower extremity amputations in patients enrolled in the Platelet Activity and Cardiovascular Events in PAD (PACE-PAD) clinical study. MACLE was measured in this group of high-risk patients after they had lower extremity revascularization (LER), procedures that open blocked arteries.
In 254 PACE-PAD patients whose platelet aggregation was measured with 0.4 μM of epinephrine, 17.5 percent showed hyperreactive platelets, and those patients with hyperreactivity had more than double the incidence of heart attack, stroke, or acute limb ischemia or major amputation within the 30 days after LER than those without hyperreactivity.
While the team has an uncommon expertise in aggregometry, and despite these learnings, their goal was to create a generalizable measure of risk that could one day be easily performed in physicians’ offices. To make global implementation feasible, the researchers designed PRESS based on a genetic signature and independent of blood collection techniques and other variables that affect aggregometry.
To create PRESS, the researchers collected platelet genetic material from 129 PACE-PAD patients before their LER procedure and designed the score based on the genetic differences seen with hyperreactivity. The researchers confirmed the score’s accuracy by checking it against platelet aggregation tests.
To further validate PRESS, the team explored the link between the score and cardiovascular risk in other patient groups. Among these was the Heart Attack Research Program, which enrolled women having coronary angiography. In this group PRESS was found to be higher in those who had a heart attack than in those with stable coronary artery disease. Among patients with lower extremity atherosclerosis followed for an average of 18 months, patients with PRESS above the middle (average) score were 90 percent more likely to have a major cardiovascular event than those below it.
“In current practice, antiplatelet therapy is not routinely recommended for the prevention of a first heart attack or stroke, but a platelet-based test would help to identify patients at highest risk, and those who would benefit most from antiplatelet therapy to prevent a cardiovascular event,” says study author Tessa J. Barrett, PhD, assistant professor in the Departments of Medicine and Pathology at NYU Langone. “Our score has the potential to further personalize cardiovascular disease risk prevention.”
Along with Dr. Berger and Dr. Barrett, study authors from the Department of Medicine were Macintosh Cornwell; Yuhe Xia; Matthew Muller; Nathaniel R. Smilowitz, MD; Jonathan Newman, MD, MPH; Florencia Schlamp; Caron B. Rockman, MD; Kelly V. Ruggles, PhD; and Judith S. Hochman, MD, director of the Cardiovascular Clinical Research Center. Also a study author was Deepak Voora, MD, of the Duke Center for Applied Genomics and Precision Medicine.
Support for this study was provided by National Institutes of Health (NIH) grants R01HL114978, R35HL144993, R01HL167917, 5R01HL118049, and K23HL150315. The NYU CTSA grant UL1TR001445 from the National Center for Advancing Translational Sciences (NCATS) partly supported the study. The NYU Langone Health DART Genomic Technology Center in Genome Technology Center is partially funded by NYU Cancer Center Support Grant NIH/NCI P30CA016087.
Media Inquiries
Greg Williams
Phone: 212-404-3500
Gregory.Williams@NYULangone.org

