Thanks to a New Treatment Strategy to Prevent Complications After a Bone Marrow Transplant, a Patient with Blood Cancer Has a Smooth Recovery

Dr. Samer Al-Homsi, director of the Blood and Marrow Transplant Program, with his patient Jack Sebastian (foreground).
Photo: Sasha Nialla
For Jack Sebastian, retirement was meant to be filled with sojourns to bed and breakfasts throughout the Northeast, and summers spent boating at the riverside cabin he shares with his sister in the Adirondacks. Instead, in January 2018, at age 65, and just weeks after saying goodbye to the Brooklyn housewares store where he had worked as a salesman, the Greenwich Village resident began feeling weak, dizzy, and short of breath while doing simple daily errands. The symptoms were surprising for a man who had enjoyed near perfect health throughout his adult life and took not a single medication.
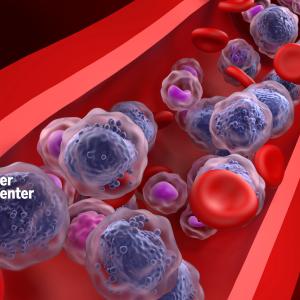
When a routine visit to Sebastian’s internist revealed that his white and red blood cell counts were low, he was referred to hematologist Bruce G. Raphael, MD, at NYU Langone Health. Concerned, Dr. Raphael performed a bone marrow biopsy. Three days later, Sebastian learned why his energy had been lagging so: he had acute myeloid leukemia, or AML. This blood cancer is caused by the rapid production of abnormal white blood cells that spread from the marrow—the soft, spongy tissue inside bones where blood cells are produced—into the bloodstream and, often, other body parts. About 11,300 people in the United States die from the disease each year, and the 5-year survival rate is only 27 percent.
“It was scary,” Sebastian says of the diagnosis. “I started thinking about everything I have: a summer place, family, strong faith, time to enjoy life. So I tried to think positively.”
Given the aggressive nature of AML, which likely would have killed him within a matter of weeks, Sebastian didn’t have much time to dwell on his situation. The next day he began a three-week inpatient stay at NYU Langone to receive chemotherapy, whose goal is to empty the bone marrow of leukemia cells and allow normal stem cells to repopulate the marrow. This prepares the patient for an allogeneic transplant, during which stem cells from a matching donor are given to the patient, thereby introducing an entirely new immune system in the patient.
“Essentially, it’s a fight between two immune systems,” says hematologist–oncologist Samer Al-Homsi, MD, director of the Blood and Marrow Transplant Program at NYU Langone’s Laura and Isaac Perlmutter Cancer Center. “The objective is to weaken the existing one and give the advantage to the new one so that it can take over and keep the leukemia in remission.”
It was Sebastian’s good fortune to have Dr. Al-Homsi in his corner. Since joining Perlmutter Cancer Center in June 2017, he has led the dramatic expansion of the Blood and Marrow Transplant Program. Within months of his arrival, the program gained membership in the National Marrow Donor Program, which operates the Be the Match Registry, a worldwide database consisting of nearly 12.5 million potential donors—a boon for patients like Sebastian, whose siblings were not viable matches. The program also became accredited by the Foundation for the Accreditation of Cellular Therapy. In addition, Dr. Al-Homsi has greatly boosted the program’s volume of autologous transplants, which use healthy stem cells from a patient’s own body to treat two other common types of blood cancer, lymphoma and multiple myeloma.
Perlmutter Cancer Center, which is designated a Comprehensive Cancer Center by the National Cancer Institute (NCI) in recognition of its top-tier research and clinical services, is on track to perform 160 transplants in 2023, nearly half of them allogeneic. “Dr. Al-Homsi has totally transformed our blood cancer program,” says Benjamin G. Neel, MD, PhD, director of Perlmutter Cancer Center.
Emblematic of that growth is an anonymous $75 million gift made in 2019 to establish the Center for Blood Cancers, which advances clinical and research efforts focused on multiple myeloma, a cancer of the plasma cells that leaves the body susceptible to infection and fractures. “This generous gift helps patients with blood cancers achieve better outcomes and advance important new research,” says Robert I. Grossman, MD, dean and CEO of NYU Langone.
Perlmutter Cancer Center, designated a Comprehensive Cancer Center by the NCI in recognition of its top-tier research and clinical services, is on track to perform 160 blood and bone marrow transplants in 2023.
Dr. Al-Homsi has already led a major research breakthrough in transplant treatment that benefited Sebastian: a new approach to fending off graft-versus-host disease, or GvHD, a medical complication in which the grafted blood and marrow cells view the recipient’s body as foreign and begin to attack it. The syndrome, which affects up to 60 percent of allogeneic transplant patients, can in its acute form cause skin rashes, liver damage, and inflammation of the intestinal tract. To prevent or at least mitigate this potentially life-threatening complication, doctors typically administer a six-month course of powerful immunosuppressants that can cause side effects, including kidney damage.
By contrast, Dr. Al-Homsi combines cyclophosphamide, an older drug that attacks the donor’s activated T cells, with a newer medication called bortezomib, which targets the dendritic cells. His phase 1 and 2 clinical trials, published in Biology of Blood and Bone Marrow Transplantation, showed promising efficacy in controlling GvHD while sparing patients the burden of traditional immunosuppressants. What’s more, the combination needs to be taken for only four days.
Sebastian completed a second course of chemotherapy, and a compatible donor was identified a month later. He returned to NYU Langone for a four-week inpatient stay. On May 24, 2018, following conditioning therapy to remove any remaining abnormal cells, he received the donor blood and marrow cells, a one-time infusion into his bloodstream that took a mere 30 minutes but effectively changed everything. “Dr. Al-Homsi and the nurses call it your new birthday,” Sebastian says of the transplant. “They gave me such hope and confidence.”
During the next several days, Sebastian felt flu-like symptoms as the new stem cells took root in his bone marrow. However, he experienced no GvHD symptoms and slowly regained strength day by day in the positive-pressure patient room, specially designed to protect people with a compromised immune system from viruses and bacteria.
After leaving the hospital, Sebastian was instructed to wear a mask in public and avoid crowded settings, such as the subway, until his immune system reconstituted. But now, his follow-up biopsies have confirmed that his old blood and bone marrow, and the deadly disease that had taken them over, are gone. “Jack is a model patient who complied with every instruction from day one,” says Dr. Al-Homsi. “He’s past the point when most relapses occur and is in great shape overall.”
Sebastian once again enjoys his summer home, where he kayaks, hikes, and takes in the glorious sunsets from his living room. “I feel like I’ve got my life back,” he says, “and that now I can do all the things I’d hoped to do in retirement.”