NYU Langone investigators look to personalize stroke prevention and treatment with advanced imaging and novel therapies.
Photo: akesak/Getty
As experts identify the mechanisms of stroke across different subtypes, NYU Langone Health researchers continue to seek new insights to enable expanded treatment, as well as more proactive prevention approaches for primary and secondary stroke. With emerging research, advanced imaging, and novel therapies, investigators aim to personalize prevention and treatment by targeting the unique origin and symptoms of stroke in each patient.
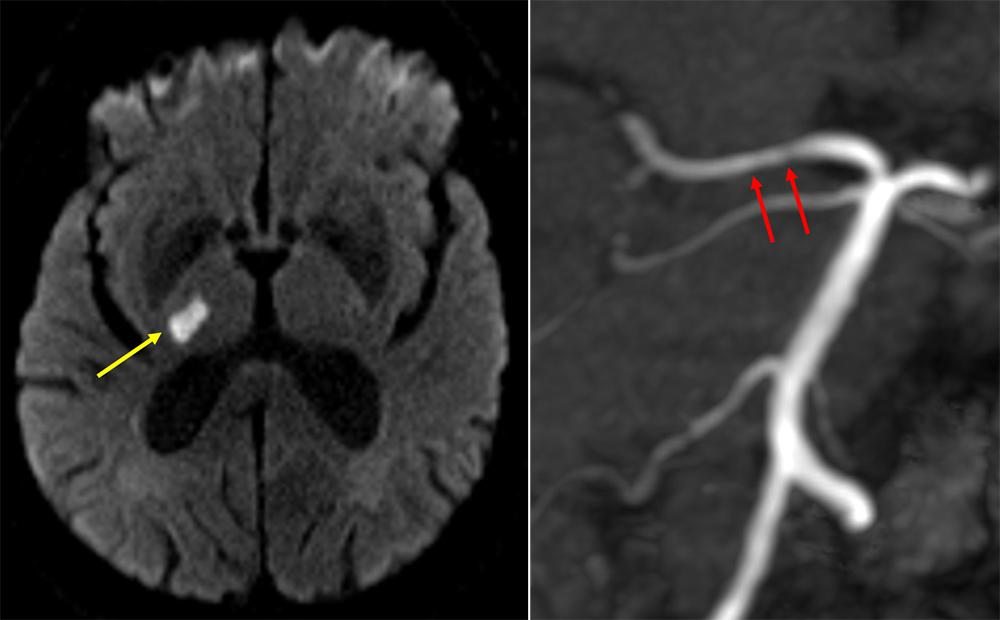
Imaging Could Shift the Center of Origin in Lacunar Stroke
Ad hoc imaging postprocessing, executed by Eytan Raz, MD, PhD, assistant professor in the Department of Radiology, is informing a new understanding of the vascular origins of lacunar strokes—small strokes that occur deep within the brain’s structures. Accounting for 15 to 20 percent of ischemic strokes, the subtype has long been thought to originate via thickening in the small arteries of the brain, due to untreated hypertension. A two-center study led by Dr. Raz and Shadi Yaghi, MD, associate professor in the Department of Neurology and research director of the Center for Stroke and Neurovascular Diseases, is investigating an alternative theory: that a proportion of these strokes may be related to atherosclerosis that lies within the larger vessel that feeds the smaller perforated vessels.
“The plaque that builds in the brain’s large artery is not often associated with narrowing, but in some patients, the plaque can expand and block off these very tiny, hair-like arteries at their origin and cause a stroke,” explains Dr. Yaghi. “It’s important to identify and treat this plaque to prevent it from blocking more of these small vessels, which may produce more pronounced neurological symptoms.”
Lacunar strokes can cause a range of symptoms depending on their involvement of the motor tract and other fibers in the brain, often causing single-sided weakness and significant long-term disability. By visualizing the smaller, more intricate vessels using high-resolution MRI sequences, Dr. Raz and Dr. Yaghi are combining their multidisciplinary expertise to pinpoint the location of lacunar strokes and gain insights that can inform treatment in the acute care setting, focus efforts to prevent a secondary stroke, and—potentially—prevent primary stroke.
“When a patient presents with a more profound stroke, we often find imaging evidence of several previously undetected silent strokes, frequently associated with mild cognitive impairment,” says Dr. Raz. “Eventually, if we can detect asymptomatic brain artery atherosclerosis at an earlier stage, aggressive intervention might prevent more significant disability down the road.”
Treatment for Post-Stroke Fatigue Could Enhance Functional Outcomes
In patients who experience profound strokes, both ischemic and hemorrhagic, sleepiness is a common and frequent barrier to positive rehabilitative outcomes. Disposition to acute rehabilitation requires patients to participate in a minimum of 3 hours of rehabilitation activities each day, a threshold reached by only 25.4 percent of patients. Thus, helping more patients—particularly younger patients poised for good outcomes—overcome lethargy and move into acute rehabilitation has become a priority for Jose L. Torres, MD, assistant professor in the Department of Neurology. His new research suggests that the novel use of the stimulant drug modafinil can help patients overcome fatigue and reach the endurance benchmark needed to qualify for acute rehabilitation care, which is associated with better functional outcomes and reduced mortality as compared with discharge to other facilities.
“Lethargy typically improves over time, but this can take several weeks to a month,” notes Dr. Torres. “The faster we can get patients to rehab, the better they do. So, I searched for an intervention that could help reduce lethargy and fatigue more quickly.”
Although amphetamine stimulants have long been tried in these patients, these stimulants are associated with harmful side effects, such as hypertension and seizures. Dr. Torres was encouraged by the documented use of modafinil, a nonamphetamine stimulant that is without side effects in patients with narcolepsy and multiple sclerosis. In a retrospective study of 199 patients, published in 2020 in the Journal of Stroke and Cerebrovascular Diseases, he and colleagues found that hospitalized stroke patients who received modafinil were more awake, more equipped to participate in physical and occupational therapy, and twice as likely to be discharged to acute rehabilitation.
Dr. Torres is working with the National Institutes of Health StrokeNet to develop a randomized, controlled trial with the potential to provide additional evidence of modafinil’s efficacy in reducing post-stroke fatigue and lethargy. He is hopeful that modafinil will expand clinicians’ available treatment options for patients and enhance the standard of stroke care.
“We’ve made a lot of progress with acute care interventions for stroke, but we still can’t help significant numbers of fatigued patients reach the milestones required for acute rehabilitative care,” says Dr. Torres. “I envision modafinil as an add-on therapy that can potentially help these patients overcome their significant lethargy and participate in the rehabilitation activities necessary for them to get better—and ultimately have improved outcomes.”