NYU Langone physicians, led by Dr. Eric K. Oermann and Dr. Daniel A. Orringer, continue to advance novel applications of artificial intelligence, with implications across the continuum of medicine.
Photo: NYU Langone Staff
With a deepening focus on unleashing novel applications of artificial intelligence (AI) across—and beyond—neurosurgery, a multidisciplinary team of physicians and mathematicians are collaborating on advanced approaches to diagnosis and patient care, developing data-driven methods that hold potential for progress across the continuum of medicine.
A Specialty Uniquely Poised to Lead with Data
Investigations into clinical applications for AI, with a focus on neurosurgical care, have gained significant momentum with the recruitment of Eric K. Oermann, MD, assistant professor in the Departments of Neurosurgery and Radiology and a leading expert in AI applications in medicine. Dr. Oermann brings deep expertise at the intersection of neurosurgery and mathematics to research projects that apply data science and algorithms to answer pressing neurosurgical questions as well as those that apply to medicine far beyond neurosurgery.
“Neurosurgery tends to be the technical spearhead of the broader medical world, innovating to benefit our own patients and medicine with a capital M,” he says. “So our discoveries in AI are at the next forefront of technological innovation in medicine, writ large.”
Dr. Oermann developed the vision for his research in close partnership with Daniel A. Orringer, MD, associate professor in the Departments of Neurosurgery and Pathology. Their combined clinical and mathematical expertise will enable them to tackle questions that neither researcher could effectively address alone. “Together we bridge the gap between science and patient care,” notes Dr. Orringer. “Our collaboration plays to Eric’s strengths as an applied mathematician, so there’s complete integration—patient to bench to computer chip to bedside.”
Gleaning More Knowledge from Fewer Inputs
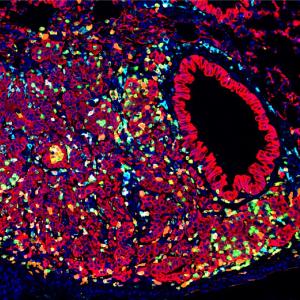
In one research vertical, Dr. Oermann is working to expand the Department of Pathology’s molecular diagnostic capacity. Building on intraoperative data gathered using stimulated Raman histology (SRH)—the laser-based imaging technique pioneered by Dr. Orringer—the new approach applies data modalities focused on maximum tumor resection and patient safety to help surgeons make more informed real-time decisions. It will enable more accurate intraoperative pathological diagnosis while reducing procedural times—ultimately increasing overall gross margins. While this research is initially focused on glioma resection, it is expected to have impact far beyond that single tumor type. “It’s really applicable to pathology affecting any organ,” notes Dr. Orringer. “We are creating a framework so clinicians can utilize algorithms to make surgeries safer and more effective.”
At the same time, Dr. Oermann is working to uncover alternative means of statistical sampling for clinical trials, using data efficiency approaches to get more scientific benefit from smaller sample sizes. One such approach, self-supervision, trains an algorithm to glean generalizable signals from the dataset itself. “This is an issue germane to neurosurgery, as there are only so many patient sets you might see in a week or a year,” Dr. Oermann notes. “But it’s really applicable to any clinical trial, which makes the solutions we’re building much bigger than the actual problems we’re solving.”
If the approach can be proved further, it could make clinical research more efficient and value driven in elucidating other rare or novel diseases like coronavirus disease (COVID-19) with smaller patient populations. “Our research related to the coronavirus is in many ways a metaphor for all of our AI work, where one clinical problem yields a mathematical project,” concludes Dr. Oermann. “The theme of our research is that we’re starting with neurosurgical problems, but in this case our approaches have proved very relevant to COVID-19—and really to medicine at large.”
Shortcutting Tumor Classification, Genetically
Dr. Oermann and Dr. Orringer are creating an algorithm to predict tumor treatment response based on genetic classification, building on previous clinical research that classified tumors into 10 categories based on molecular characteristics. The AI approach may ultimately circumvent the need for traditional genetic testing to determine tumors’ specific mutations.
“There’s a growing acceptance that genetics most efficiently predicts prognosis in response to treatment,” says Dr. Orringer. “Many of these mutations are associated with a phenotype, and we can train algorithms to identify these based on morphologic changes, intraoperatively, in a fraction of the standard time.”
“This AI-based approach has the potential to fuel personalized medicine in a way that simply wasn’t conceivable in the past.”—Eric K. Oermann, MD
Equipped with this information at the time of surgery, clinicians can make more targeted decisions. A tumor identified as benign with a good surgical prognosis, for example, could be aggressively treated, ensuring full resection when safe. In addition, clinical trials for brain lesions increasingly incorporate an intraoperative component, so patients could potentially receive a novel agent in trial during surgery, driven by advances in AI-based diagnosis.
“This AI-based approach has the potential to fuel personalized medicine in a way that simply wasn’t conceivable in the past,” adds Dr. Oermann.
Building Efficiencies into Spine Care
An AI-assisted platform for spine surgery, currently under development, will subsume methods to stratify risk, predict outcomes, and prevent complications by guiding decision-making, optimizing patient workflow, and applying advanced imaging.
Dr. Oermann is investigating the use of AI in reconstructing CT scans based solely on MRI or in-office, three-dimensional EOS radiography, both to enhance care and to reduce unnecessary radiation exposure. “This would be a game changer for taking care of our spine patients,” he says. “They’d come with the existing imaging and we’d virtually conjure up the CAT scan without an additional trip or extra imaging for the patient.”
AI-enabled efficiencies are also under investigation for endovascular surgeries. Focal robotic applications have the potential to reduce surgical time and enhance precision by automating discrete techniques, such as a translabyrinthine approach—reduced to five minutes from an hour or more—as well as by placing instrumentation, such as pedicle screws, in the spine. “You have a pedicle, which is a circular tube, and the directions are forward, backward, rotate. It’s a simple neurosurgical problem that we’ve translated into an engineering problem, which becomes a mathematical problem and solution,” notes Dr. Oermann.
AI-Informed Cross-Campus Collaborations
In two projects with the NYU Center for Data Science, the team is investigating the application of AI to surgical endoscopy and to decoding signals from the human brain. The latter project, which Dr. Oermann has been working on for years, is developing tools for reverse engineering microprocessors that the team hopes will be immediately applicable to reverse engineering neural circuitry as well. “The beauty of mathematics is its universality. We believe that the techniques we develop for reverse engineering computers may one day be helpful for reverse engineering the human brain,” says Dr. Oermann.