Richard P. Novick, MD
Photo: Mike Weymouth
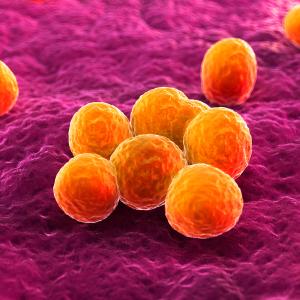
Genomic “islands” that evolved from viruses can be converted into “drones” that disable Staphylococcus aureus, the sometimes-deadly bacterial infection that is resistant to antibiotics and a threat to safe hospital care, a new study finds.
Conducted by researchers from NYU School of Medicine and published online in the journal Nature Biotechnology on September 24, the study found that a certain type of bacterial DNA can be engineered to replace genes that help these microorganisms cause disease with genes that instead kill or cripple bacteria.
The type featured in the study, a “pathogenicity island,” evolved from viruses that stayed permanently in the bacteria they infected to become a part of their genetic system. The result is a hybrid entity that contains useful genes passed on by the bacteria when they reproduce, but that is also in some cases cut out of the bacterial superstructure, and packaged like a virus in a protein shell (capsid) that can inject its DNA into other bacterial cells.
This mix of evolutionary leaps has fashioned genomic islands as perfect drone-like vehicles to deliver genetic payloads throughout bacterial populations, say the study authors. When injected into mice with an otherwise lethal staph infection, the research team’s engineered S. aureus pathogenicity islands (SaPIs) killed the bacteria and rescued the treated animals.
“Given efficacy seen so far, and the safety record of related treatment attempts, we are getting set to test our drones against a staph infection that interferes with milk production in cattle, and if successful there, in humans with staph infections,” says senior study author Richard P. Novick, MD, the Recanati Family Professor of Science at the Skirball Institute of Biomolecular Medicine within NYU School of Medicine, and a member of the National Academy of Sciences.
“It is an extraordinarily rewarding experience to spend a long career studying an infection, and then to arrive at a potentially new way to treat it,” says Novick, who earned his MD at NYU School of Medicine and has been studying staph since.
One-third of the human population are carriers of S. aureus, generally without symptoms. But those with weakened immune systems may develop life-threatening infections in the bloodstream, lungs (pneumonia), or organs (sepsis). S. aureus has long posed a threat in hospitals, where there are numerous surfaces for bacteria to colonize, and has more recently become a growing problem in the community (e.g., gyms, playgrounds, schools, military barracks, and doctors’ offices).
In addition, antibiotics used against staph are ineffective because an increasing number of strains have become resistant to these drugs. With many staph infections now untreatable after decades of antibiotic overuse, the field urgently seeks new ways to counter infections.
Borrowing Viral Tricks
It was during research in the 1980s on a gene called TSST1—which causes a dangerous complication of staph infections called toxic shock syndrome—that Novick and colleagues first discovered that a pathogenicity island carried TSST1 as part of its cargo. The team’s subsequent drone design effort grew from the understanding that staph bacteria depend on genomic islands to share useful genes. In this way, an entire population benefits when any one cell stumbles on a change that helps it to survive, and not just its offspring.
“The natural role of islands in such gene transfers set them up as a new treatment approach, if they could be made to contain genes that hampered bacteria instead of encouraging infection,” says Hope Ross, PhD, a longtime member of the lab. In 2013, it was Ross that first saw this potential, and suggested that the lab focus on it.
While pathogenicity islands can spread like viruses under certain conditions, they have lost a large portion of their ancestral, viral DNA via genetic accidents, and so are smaller. In designing their drone, the team took advantage of this to package islands in protein shells the size of those used by larger intact viruses, which left space for the addition of antibacterial genes.
As a first test, the team added to their island a CRISPR/Cas9 sequence, a genetic system that targets and cuts the DNA chain within a targeted gene, a lethal event in bacteria. Another drone studied by the team contains a gene for the enzyme lysostaphin, which directly kills bacteria by breaking down their cell walls. The team also studied a CRISPR approach with the potential to disable several, disease-causing bacterial genes without killing the bacteria, which promises to prevent infections from becoming drone resistant.
Novick’s study also led to another important conclusion. “The drone system would not, like antibiotics, disrupt patients’ microbiomes, the mix of bacteria in the gut, some species of which are essential to digestion and to general health,” he says.
Along with Novick and Ross, authors of the study were Geeta Ram, Ivelisse Rodriguez-Pagan, and Dun-Rong Jiang in the Department of Microbiology and Department of Medicine at NYU School of Medicine. This work was supported by NIH grant R01-AI22159, and a grant-in-aid from NYU School of Medicine. A patent application has been filed by Dr. Ram, Dr. Ross, and Dr. Novick on the basis of the study results.
Media Inquiries
Greg Williams
Phone: 212-404-3500
gregory.williams@nyulangone.org