Photo: Callista Images/Getty
Advances in treatment have led to the largest yearly declines in deaths due to melanoma ever recorded for this skin cancer, results of a new study suggest.
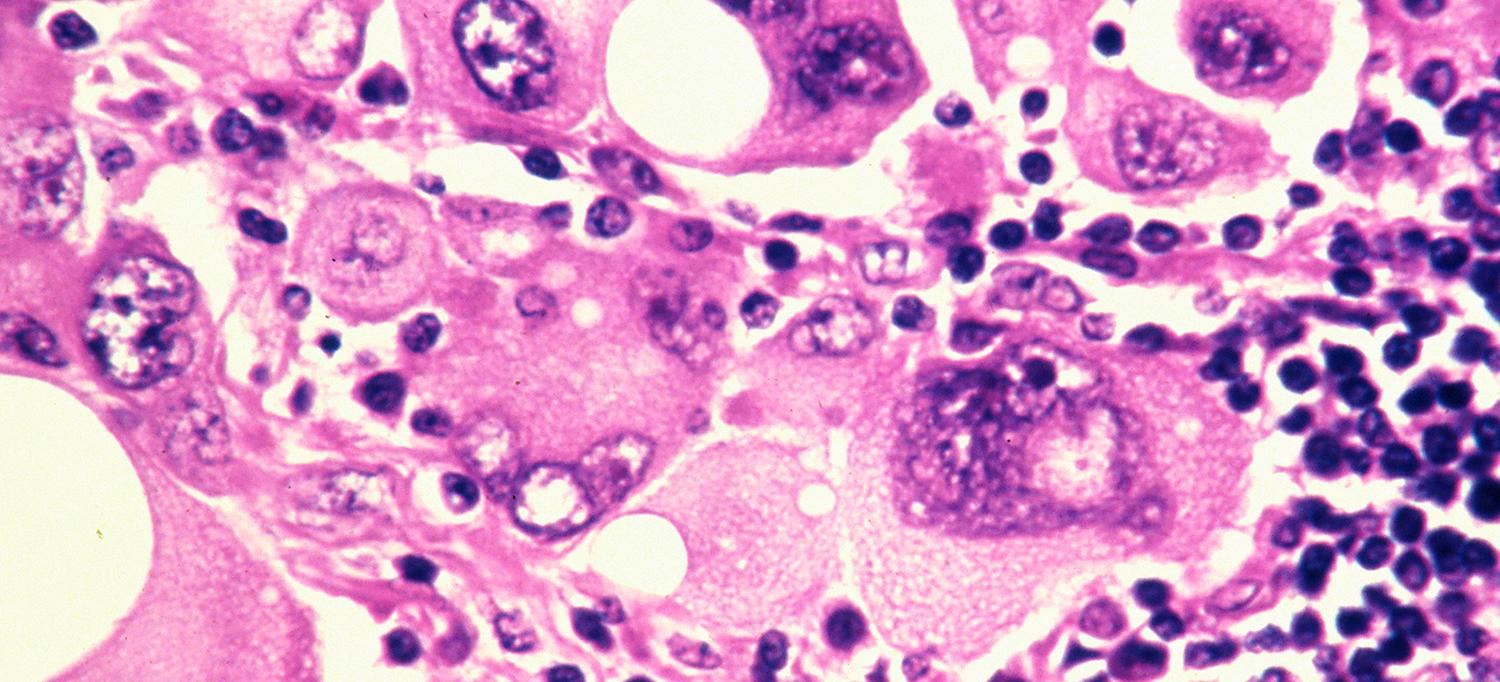
Led by researchers at NYU Grossman School of Medicine, NYU Langone’s Perlmutter Cancer Center, and Harvard University, the study showed that death rates among white Americans—the group that accounts for almost all cases—climbed 7.5 percent between 1986 and 2013, but then dropped by nearly 18 percent over the next 3 years. The death rates were for metastatic melanoma, the aggressive form that spreads from the skin to other organs, such as the lung, liver, or brain.
The authors say the size of the declines outstrip comparable decreases in cancers of the prostate, breast, and lung. They also note that the unrivaled drop in melanoma deaths coincided with the introduction of 10 new therapies for the skin cancer. These treatments either harness the body’s immune system to fight the disease or directly target melanoma cells that have a specific gene mutation.
“Our findings show how quickly patients and physicians accepted these new drugs because they profoundly reduce deaths from melanoma,” says co-senior study author David Polsky, MD, PhD. “These therapies are now considered the backbone of how we treat this cancer,” says Dr. Polsky, the Alfred W. Kopf, MD, Professor of Dermatologic Oncology at NYU Langone Health and Perlmutter Cancer Center.
The report, published online March 19 in the American Journal of Public Health, is the first to highlight the role of these new drugs in helping Americans survive melanoma, says Dr. Polsky, who is also a professor in the Department of Pathology at NYU Langone.
According to some estimates, melanoma is among the most common forms of cancer in the United States, with about 100,000 new cases occurring every year. Melanoma has been notoriously difficult to treat after tumors spread throughout the body, and conventional treatment methods such as chemotherapy have limited effect against the disease. While the specific causes of melanoma are unclear, genetics and exposure to ultraviolet (UV) radiation in sunlight and tanning beds are known to increase risk, particularly among fairer-skinned people.
The newer therapies, which came into use in the last decade, are far more effective and less toxic than standard chemotherapy, but are much more expensive, the investigators say. The drugs fall into two broad categories: those that target the BRAF gene, which is mutated in a little less than half of melanoma patients; and immune checkpoint inhibitors, which prevent melanoma tumors from tricking the immune system into ignoring the cancer.
How the Study Was Conducted
For the study, researchers analyzed new cases and deaths from melanoma collected by the National Cancer Institute and the Centers for Disease Control and Prevention. These numbers spanned from 1986 to 2016 and involved nearly a million Americans. Dr. Polsky notes that the steep drop in deaths cannot be readily explained by better detection methods, because death rates dropped sharply, rather than steadily over time. In addition, many healthcare groups have been pushing for early detection exams since the 1980s, so the timing of these declines matches up better with the introduction of the new therapies.
Nevertheless, the researchers caution that early detection is still important, allowing for less toxic forms of treatment and lowered healthcare costs. They emphasized that prevention, avoiding excessive UV light exposure, and promptly seeking medical care when there is a change in the skin’s appearance, are crucial to reducing the risk of developing metastatic melanoma.
Dr. Polsky says future studies should investigate socioeconomic factors that may affect access to the newer therapies, as well as the effect of these treatments on other ethnic groups.
Funding for the study was provided by NYU Langone, where other investigators involved in the study are Jennifer A. Stein, MD, PhD, and Jeffrey S. Weber, MD, PhD. Alan C. Geller, MPH, RN, at Harvard University in Boston is the other senior co-investigator of the study. Juliana Berk-Krauss, MD, at State University of New York (SUNY) Downstate in Brooklyn, is the study lead investigator.
Media Inquiries
Shira Polan
Phone: 212-404-4279
shira.polan@nyulangone.org