The immunotherapy drug nivolumab is safer and more effective than ipilimumab—the current standard of care—in treating patients with resected stage III and stage IV melanoma, according to an international clinical trial led by a researcher from NYU Langone Health’s Perlmutter Cancer Center.
Principal investigator Jeffrey S. Weber, MD, PhD, professor of medicine at NYU School of Medicine and deputy director of Perlmutter Cancer Center, presented the findings September 11 in Madrid, Spain at the annual meeting of the European Society for Medical Oncology. The results of this study were also published simultaneously in the September 11 online version of the New England Journal of Medicine.
The study compared the 2 drugs in 906 patients with stage IIIb, IIIc, and IV melanoma. All participants had the disease surgically removed prior to receiving immunotherapy, making this study one of the first to investigate these very high-risk patients in a head-to-head trial. The study involved 2 groups of 453 participants–one treated with nivolumab and the other treated with ipilimumab.
VIDEO: Dr. Jeffrey Weber explains the key findings of an international clinical trial comparing nivolumab and ipilimumab, which show the superiority of nivolumab in effectiveness and safety.
After 12 months of continuous therapy, 71 percent of patients treated with nivolumab lived without recurrence of the disease, compared with 61 percent of those treated with ipilimumab. At 18 months, the relapse-free survival rate for nivolumab was 66 percent, while it was only 53 percent for ipilimumab. This international trial was conducted at 130 medical centers across 25 different countries.
“Our results demonstrate that nivolumab is more effective in treating patients with stage III and IV melanoma, cutting the risk of relapse by a third,” Dr. Weber says. “Results like this will change how we practice medicine. Hopefully, physicians will embrace the use of nivolumab in these high-risk patients as adjuvant therapy.”
Nivolumab, publicly marketed as Opdivo®, also was more tolerable for patients than ipilimumab. Only 14 percent of patients treated with nivolumab experienced severe side effects while 45 percent of patients experienced them with ipilimumab. Some patients had to discontinue treatment due to the severity—but only 5 percent of those on nivolumab, as opposed to 31 percent of those on ipilimumab. The most common side effects for both therapies were fatigue and diarrhea.
“The safety of nivolumab is very promising,” Dr. Weber adds. “Compared with the high toxicity of ipilimumab, it is much more tolerable for the patients. Given its tolerability, combined with its efficacy, nivolumab could realistically become the new standard of care for adjuvant melanoma treatment.”
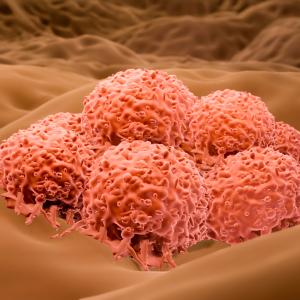
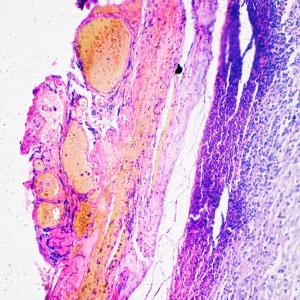
Metastatic melanoma accounts for approximately 1 percent of skin cancer cases, but, at the same time, causes the majority of skin cancer deaths. Nivolumab and ipilimumab are already approved by the U.S. Food and Drug Administration for the treatment of metastatic melanoma; for some patients, the two drugs have been used in combination.
Dr. Weber says that he hopes to lead further research that looks at categorizing tumors that occur in relapsed patients and studying whether or not they would benefit from another resection and more nivolumab. He also says that more studies are needed to examine why some patients relapse following treatment and others do not.
“Knowing that nivolumab is more effective and safer than ipilimumab as adjuvant therapy will change how we treat this fatal disease,” Dr. Weber concludes. “I predict that fewer people will die from metastatic melanoma in the next decade compared to the last because of therapies like nivolumab.”
Bristol-Meyers Squibb, the manufacturer of both nivolumab and ipilimumab, funded this clinical trial and provided Dr. Weber and his colleagues with research support.
Media Inquiries
Jim Mandler
Phone: 212-404-3525
jim.mandler@nyumc.org
Jeffrey Molter
Phone: 212-263-9423
jeffrey.molter@nyumc.org