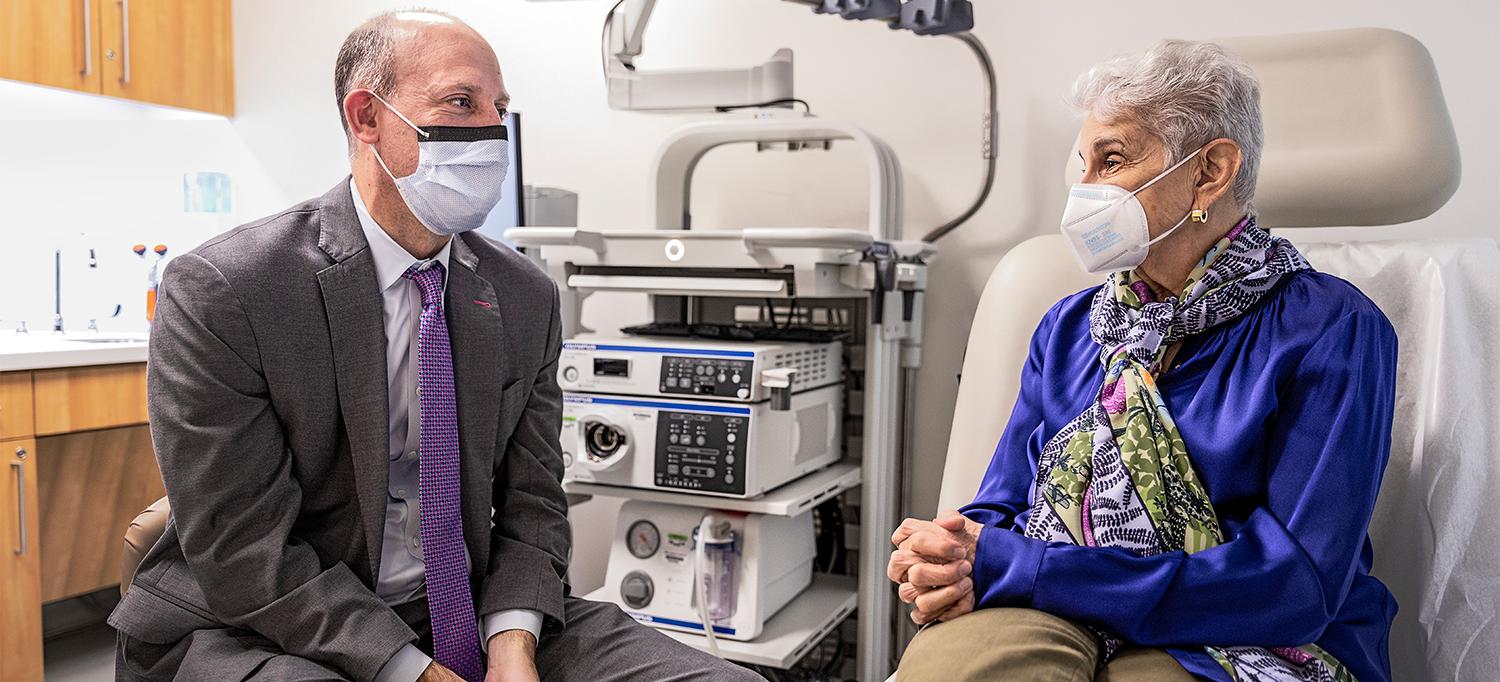
Rosalie successfully manages ulcerative colitis with a multidisciplinary team of healthcare providers, including inflammatory bowel disease expert Dr. David P. Hudesman.
Photo: NYU Langone Staff
For more than two decades, Rosalie managed ulcerative colitis, a type of inflammatory bowel disease (IBD), with oral medications and, on occasion, suppositories or enemas to quiet minor flare-ups. That regimen kept symptoms in check until, at age 57, she landed in the hospital—a sign of her worsening condition.
After being treated and released, Rosalie stayed on the same medicines she had been taking all along. But a few years later, she experienced another major flare-up, the worst she had ever had up until that point. “When I say major, I couldn’t leave the house,” she explains. The litany of symptoms, including bleeding, cramping, and diarrhea, made her miserable.
Following a colonoscopy, which revealed the severity of the situation, Rosalie’s gastroenterologist referred her to the experts at NYU Langone’s Inflammatory Bowel Disease Center. It marked a turning point in the trajectory of her health.
VIDEO: Rosalie discusses having ulcerative colitis and how the Inflammatory Bowel Disease Center team has helped improve her quality of life.
Help for Ulcerative Colitis
From that first visit with David P. Hudesman, MD, a gastroenterologist and the center’s co-director, Rosalie felt at ease. Their meeting, which included detailed questions about her medical history, “just made me feel so understood, and his attitude was so encouraging.”
Rosalie had been reluctant to go on a biologic, a class of therapeutics made from live organisms. Biologics block proteins that cause inflammation in the gut. A few biologics are considered first-line therapy for treating moderate to severe ulcerative colitis. But some are linked to a small risk of certain cancers. As a breast cancer survivor, Rosalie appreciated that Dr. Hudesman listened to her concerns, walked her through the benefits and risks, and clearly explained how the biologic he intended to prescribe would work.
“The bottom line is…everybody listens, and that is critical.”—Rosalie, Age 75
The first therapy he prescribed did the trick, for a while, at least, and when it no longer kept symptoms from flaring, he switched her to a different one. Without biologic therapy, Rosalie is certain she would have been a candidate for surgery.
Today, the 75-year-old retiree is a regular at the Inflammatory Bowel Disease Center, where she goes for injections every 8 weeks. It’s where she sees Dr. Hudesman, his “kind, compassionate” physician assistant Juliette A. Bender-Heine, PA, and a team of nurses who, in her words, are “friendly and efficient.”
One-Stop Comprehensive Care for IBD
Few places in the country bring together the breadth of services and world-class expertise that the Inflammatory Bowel Disease Center offers under one roof. Patients benefit from access to a multidisciplinary team providing an array of treatments, including gastroenterology services, infusion and injection therapies, surgical consultations, ostomy care, nutritional support, and psychosocial care.
Every other week, Rosalie attends a support group led by clinical psychologist Jessica A. Gerson, PhD, for people with IBD. The group itself provides a community for sharing and learning from others about their IBD experiences. Rosalie also sees Dr. Gerson every month for individual therapy. Through those sessions, she has learned relaxation techniques and other strategies that help with reducing stress—which can worsen ulcerative colitis symptoms—and with managing symptoms when they do arise.
People with IBD often experience anxiety or depression, or both, because these illnesses can impact quality of life, Dr. Gerson explains. “Learning new coping techniques can be a great help,” she says. In addition, research into the gut–brain connection suggests that reducing stress can aid in physical healing and help stave off flares. Through the Inflammatory Bowel Disease Center, people can participate in short-term individual therapy, support groups, gut-directed hypnotherapy groups, and cognitive-behavioral therapy groups, as well as a buddy—peer-to-peer—program.
Navigating dietary restrictions poses another challenge for people with IBD. Every month, Rosalie sees Arielle Leben, MS, RD, CDN, a registered dietitian with the Inflammatory Bowel Disease Center, who “has given me the tools that I need to manage flares on my own.”
Leben works one-on-one with people to develop personalized nutrition plans. This equips them to manage their diets depending on the circumstances—for example, whether they are having a flare, preparing for or recovering from surgery, or in remission.
“One of the goals of the nutrition program is to foster a healthy relationship with food,” adds Leben. When counseling patients, she places as much emphasis on what people should be eating to manage symptoms and optimize overall health as she does on what to avoid or limit.
From Rosalie’s point of view, dealing with ulcerative colitis can be isolating, painful, and debilitating, but having a support system to help manage the physical and mental effects has made all the difference. “I’m the poster child for the Inflammatory Bowel Disease Center; it is an absolutely remarkable place for people with this illness,” she says.

