Findings Advance Efforts to Identify Who Would Benefit from More Aggressive Therapy at Earliest Stages
In what is believed to be the largest epigenetic analysis to date of cell-signaling molecules in early-stage melanoma, researchers at NYU Langone Medical Center and its Laura and Isaac Perlmutter Cancer Center have identified two tiny bits of non-coding genetic material in primary tumors that appear critical to stalling the cancer’s spread—and essentially setting the biological fate of the disease.
Reporting in the Journal of the National Cancer Institute online Feb. 11, researchers say that pinpointing these so-called “microRNAs” — known as miR-382 and miR-516b — could provide the basis for future medical tests that identify those melanoma most likely to spread and kill. In fact, the NYU Langone team that led this study has already begun a follow-up clinical study to see if any microRNAs have a similar prognostic value in identifying melanoma patients whose cancer is more likely to spread to the brain. Nearly half of people who die from melanoma succumb from its spread to the brain, they note.
MicroRNAs are epigenetic factors, chemical cousins of DNA that help regulate gene function. But unlike other kinds of RNA, microRNAs do not get translated into specific proteins.
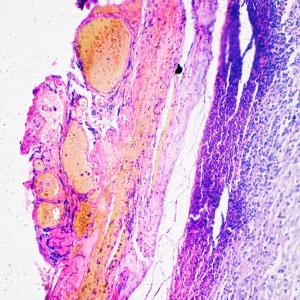
Detection of the suppressor microRNAs emerged from the analysis of more than 800 of them found in tumor tissue samples from 92 men and women with melanoma. Some 48 of the patients had aggressive cancer, while the rest did not. Tumor tissue samples were provided by patients who agreed to donate their specimens to a research database maintained at NYU Langone.
“Our study results show the suppressive effects of two specific microRNAs in melanoma that are less active in aggressive, primary tumors,” says cell biologist and senior study investigator Eva M. Hernando-Monge, PhD. “Going forward, our goal is to show how we can use this information to identify patients more at risk of aggressive disease, and see whether early, more intense therapy improves survival from melanoma,” says Hernando, an associate professor at NYU Langone and its Perlmutter Cancer Center.
The American Cancer Society estimates that in 2015, some 73,870 new cases of melanoma will be diagnosed in the United States, resulting in close to 9,940 deaths.
According to oncologist and study co-investigator, Iman Osman, MD, a professor in the Ronald O. Perelman Department of Dermatology at NYU Langone and an associate director of the Perlmutter Cancer Center, “Now that we know that the fate of these melanoma tumors is set and predetermined by these microRNAs, we can investigate whether the same principle applies in other tumors and what interventions are possible to prevent or stall their predestined spread.”
As part of the study, researchers focused their analysis on 40 microRNAs found active or inactive in early-stage tumors, which had also grown deeper than 2 millimeters and were, as a result, already known most likely to spread. Further experiments were designed to show which, if any, of the microRNAs hindered or helped cancer spread among cells grown in the lab. This helped narrow the search to just a few microRNAs. When the scientific team compared their microRNA results to active or inactive microRNAs in an additional set of tissue samples from 119 people with early-stage melanoma, only the two microRNAs stood out as less abundant in localized cancers that did not spread.
Moreover, the researchers report, injections in mice of human melanoma cells programmed to over-activate either miR-382 or miR-516b successfully blocked cancer spread, while injections of melanoma cells with no changed microRNA activity produced significant cancer spread.
Funding support for the study was provided by the National Cancer Institute, part of the National Institutes of Health, and grants R01 CA155234, T32 CA009161-37, P30 CA016087-30, P30 CA016087-32, C026719, and the Marc Jacobs campaign to support melanoma research.
Besides Osman and Hernando, other researchers involved in the study were lead study investigator Doug Hanniford, PhD; Miguel Segura, PhD; Judy Zhong, DPhil; Elliot Philips; Xavier Jirau-Serrano; Farbod Darvishian, MD; Russell Berman, MD; Richard Shapiro, MD; and Anna Pavlick, DO. Additional research support was provided by Brian Brown, PhD, at Mount Sinai, also in New York.
Media Inquiries
David March
Phone: 212-404-3528
david.march@nyulangone.org