In the years after she was diagnosed, Lauren Mims had five surgeries to remove her fibroids, but they grew back every time.
Credit: Sanjay Suchak
Lauren Mims started getting routine iron infusions at the age of 17 to combat severe anemia caused by her heavy menstrual cycles.
“I remember by the time I got to graduate school—all PhD students are tired—but I was really tired,” Mims said. “One day I fainted on the way to class and ended up seeing a hematologist. They did scans and tests, and that was the first time I was diagnosed with fibroids.”
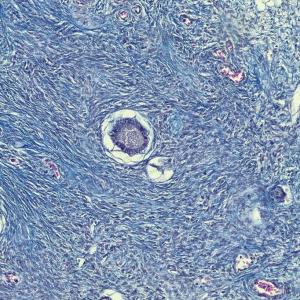
Fibroids, benign tumors that grow on the smooth muscle of the uterus, cause a variety of symptoms, including heavy bleeding, anemia, pelvic pain, pelvic pressure, urinary frequency, constipation, and painful sex. Between 70 to 80 percent of all women have fibroids. Incidence rates are higher among Black women and women with a family history of the condition.
In the decade following her diagnosis, Mims had five surgeries to remove dozens of fibroids, but they grew back aggressively after each procedure. She continued to require iron infusions every three to six months.
When she moved to New York, Mims, now a professor of applied psychology at New York University, sought care from Taraneh Shirazian, MD, director of NYU Langone Health’s Center for Fibroid Care and associate professor in the Department of Obstetrics and Gynecology at NYU Grossman School of Medicine.
“She said, ‘There’s no reason that fibroids should be disrupting your life, and I am going to do something to change it,’” Mims recalled.
NYU Langone gynecologists treat fibroids with medications, nonsurgical treatments, and surgical approaches designed to resolve symptoms and restore quality of life. Dr. Shirazian recommended a comprehensive approach that involved three treatments in one surgery: hysteroscopic removal of fibroids, placement of an intrauterine device (IUD), and transcervical fibroid ablation, one of the newest tools in fibroid treatment. This technique uses radiofrequency energy to destroy fibroid tissue while preserving the uterus.
“You place a tiny probe into the center of the fibroid using visual guidance from an ultrasound,” explained Dr. Shirazian. “The probe delivers radiofrequency, which is heat. The heat helps the fibroid shrink over the course of time, typically three to six months, and it will help the heavy bleeding and other symptoms such as pelvic pain and pressure.”
This minimally invasive procedure has allowed Mims to return to work with newfound energy, alleviated her symptoms, and eliminated the need for iron infusions.
“It wasn’t until I have now gone about 10 months without these life-altering symptoms that I realized how many things were tremendously impacted because of this disease,” Mims said. “I was very close to getting a hysterectomy because I had had so many surgeries, and I had been in the ER so many times receiving infusions to stop bleeding, to replenish blood cells, and I was tired of just living very sick. This is the first stretch of my life that I haven’t felt that way, which is really amazing.”
Recent survey data from The Harris Poll highlighted a concerning trend: many women, including a quarter of those ages 18 to 34, believe hysterectomy, removal of the uterus, is the sole option for fibroid management.
Dr. Shirazian and the team of specialists at the Center for Fibroid Care emphasize that a spectrum of solutions exists to address fibroid symptoms effectively and preserve fertility when desired.
“As a leading center for fibroid treatment, we prioritize empowering patients with comprehensive information and modeling best practices for providers around the country,” said Dr. Shirazian. “Every woman deserves to know her options and make informed decisions that enhance her quality of life.”
Watch more on CBS Mornings.