Combining diagnostic and surgical teamwork, Center for Esophageal Health experts perform an advanced workup and revisional surgery to resolve choking symptoms for a patient with a history of gastroesophageal reflux disease.
Photo: ChrisChrisW/Getty
Guided by advanced esophageal physiology diagnostics, surgeons at NYU Langone’s Center for Esophageal Health successfully performed robotic revisional surgery on a 54-year-old woman who presented with debilitating symptoms, including “stabbing pain after meals,” choking, dysphagia, and daily heartburn unresponsive to medical therapy.
The woman had a history of gastroesophageal reflux disease (GERD), for which she had surgery several decades earlier, and was taking immunosuppressant therapy for Crohn’s disease. Previous procedures to dilate her upper esophagus had failed to relieve symptoms of dysphagia and choking, which were severely interfering with her quality of life and had forced her to take a leave of absence from her job as a teacher.
Previous Efforts Fail to Relieve Symptoms
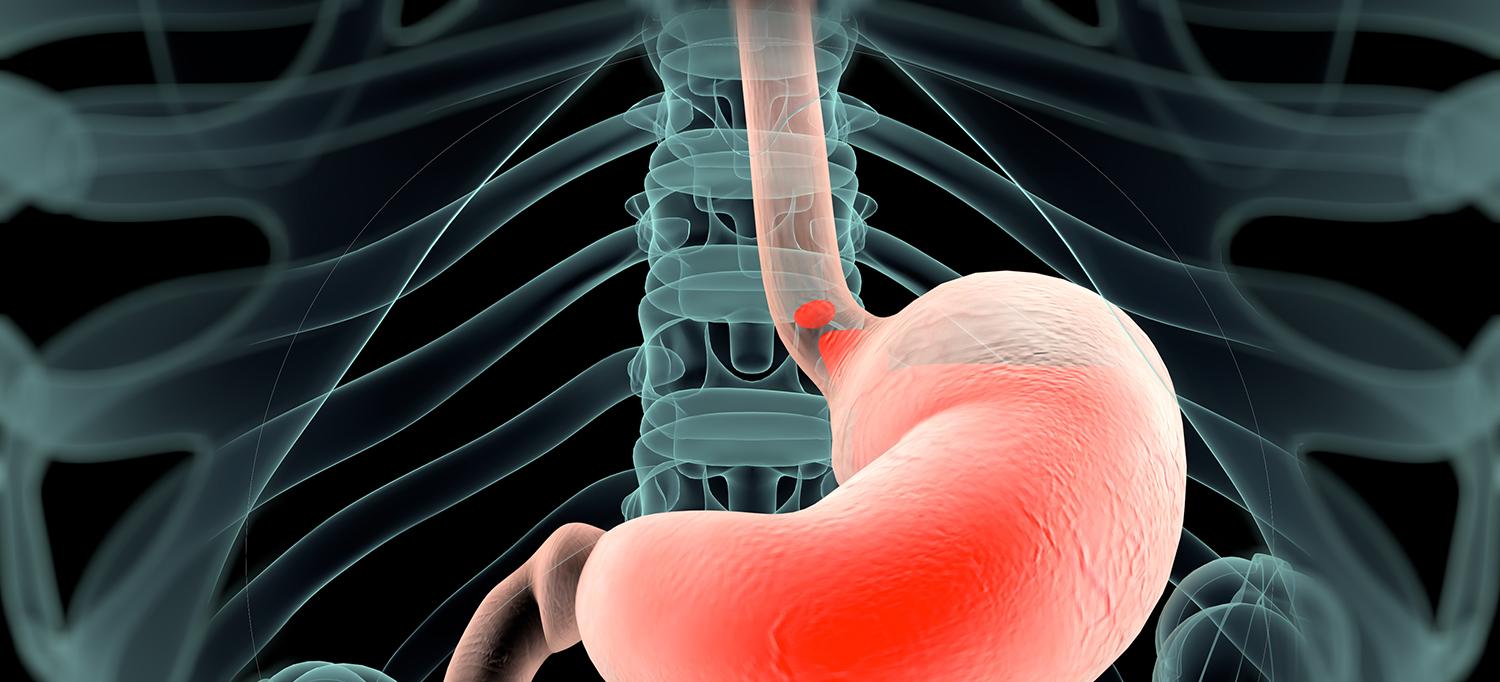
While in her early 20s, the patient had an open Nissen fundoplication surgery using a 9-in incision for GERD, a procedure that wraps the stomach completely around the lower esophagus to create a new functional valve preventing reflux. Endoscopic studies performed before she was seen at NYU Langone suggested that a stricture or narrowing had developed in her lower esophagus with upstream dilation and tortuosity of the esophagus, accompanied by a paraesophageal hernia. Her referring doctors outside of NYU Langone had also considered a diagnosis of achalasia, a disorder associated with narrowing that impedes the ability of the esophagus to contract and relax appropriately during swallowing. Several endoscopic-guided dilations were attempted in an effort to stretch her esophageal passage, but the procedures failed to resolve her symptoms.
The patient was advised against surgery due to prior open surgery causing significant adhesions and the risks of inadvertent injury to the esophagus, stomach, or vagus nerves in the presence of extensive scar tissue. The woman was also taking immunosuppressive medications for Crohn’s disease—including high doses of aminosalicylates and infliximab—which increase the risks of postsurgical infection and impaired wound healing. At a crossroads, she then sought a second opinion at NYU Langone.
NYU Langone Performs Advanced Workup
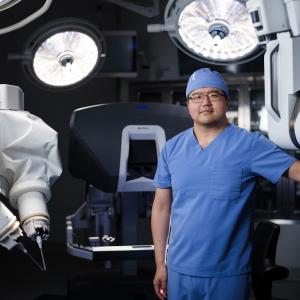
The patient scheduled a consultation with Tanuja Damani, MD, surgical director of the Center for Esophageal Health and associate professor in NYU Langone’s Department of Surgery. Dr. Damani conferred with Abraham R. Khan, MD, the center’s medical director and assistant professor in the Department of Medicine, who specializes in neurogastroenterology and motility disorders of the gastrointestinal (GI) tract.
The NYU Langone team conducted an extensive workup. First, Dr. Khan did a detailed assessment of the patient’s esophagus using a functional lumen imaging probe (FLIP), a minimally invasive device that simultaneously measures the diameter and contractility of the esophagus under a sedated upper endoscopy. The diagnostic evaluation revealed a likely extrinsic obstruction at the junction where the esophagus joins the stomach, preventing the lower esophageal sphincter from opening appropriately.
The findings did not support a diagnosis of achalasia and instead singled out a paraesophageal hiatal hernia as the root problem. “Our workup also eliminated the need to perform an esophageal manometry, one of the standard tests done to exclude achalasia,” notes Dr. Khan, “which would have been particularly difficult and uncomfortable in this case as it requires the patient to be awake during placement of an intranasal catheter to assess swallowing function, and she had an obstructed lower esophagus.”
Robotic Surgery Repair Leads to Successful Outcome
With a specific diagnosis in hand, Dr. Khan and Dr. Damani recommended proceeding with robotic revisional surgery. Although minimally invasive revisional surgery after prior open surgery carries risks, they are significantly mitigated in high-volume centers like NYU Langone where surgeons have extensive experience and expertise in revisional foregut and complex robotic procedures.
“We also considered that previous attempts to control her symptoms with medications and endoscopic procedures had failed,” says Dr. Damani. “At the same time, the symptoms had become debilitating and were severely curtailing her ability to enjoy food and pursue her daily activities. Revisional surgery was clearly the best way to address the root cause of her problems.
Dr. Damani performed a robotic repair of the paraesophageal hernia, using biodegradable mesh to reinforce the hiatal opening at the diaphragm and prevent postoperative recurrence. They then took down the existing Nissen fundoplication, which involves a complete 360-degree wrap of the stomach around the esophagus, and converted it to a Toupet fundoplication, a partial 270-degree wrap.
The Toupet method is often preferred for patients who have persistent dysphagia as well as reflux, as it does not completely encircle the esophagus. Thus it causes less postoperative side effects of dysphagia and gas bloat syndrome and allows the patient’s natural gastric venting functions, such as belching and vomiting. In addition, it has been shown in studies objectively and subjectively to provide the same reflux control as a Nissen fundoplication.
The patient was extremely pleased with the successful outcome. “After less than 48 hours in the hospital, she was able to return home and eventually resume teaching,” says Dr. Damani. “Thanks to the advanced expertise in esophageal testing and robotic surgery we have at NYU Langone, this patient was able to embark on a new course of treatment that significantly improved her quality of life.”