Thoracic Surgeons & Pulmonologists Play Critical Role in Caring for Patients with Coronavirus on Ventilators

Robert J. Cerfolio, MD, director of clinical thoracic surgery and chief of hospital operations, has developed a rigorous protocol to enable doctors to perform bronchoscopies while preventing the spread of COVID-19.
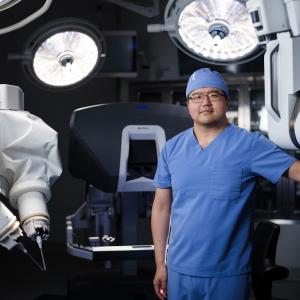
Photo: NYU Langone Staff
By the second week of April, the number of critically ill patients with coronavirus disease (COVID-19) at NYU Langone Health has reached its spring peak. Among those in the first row of the front lines are the pulmonologists and thoracic surgeons, who perform bold interventions to help patients in severe respiratory distress. “They have implemented several key clinical strategies that greatly improved outcomes,” notes Aubrey C. Galloway, MD, the Seymour Cohn Professor of Cardiothoracic Surgery and chair of the Department of Cardiothoracic Surgery.
One important contribution is an innovation that sprang from Luis F. Angel, MD, an interventional pulmonologist who is medical director of lung transplantation, and Zachary N. Kon, MD, a cardiothoracic surgeon who is surgical director of lung transplantation.
Most patients with COVID-19 who are admitted to NYU Langone’s intensive care units are placed on mechanical ventilation. To say that experience is unpleasant is an understatement. First, the hookup requires the insertion of a breathing tube snaked down the patient’s throat, which is anchored inside by an inflatable cuff. The choking sensation is so strong that patients require heavy sedation to prevent them from yanking the tube out.
Complicating matters, some COVID-19 patients require ventilation for weeks. In these cases, doctors would typically recommend a tracheostomy to connect the ventilator tubing to a surgically created opening in the windpipe, bypassing the mouth and throat. This configuration is far more comfortable for the patient and requires less sedation but unfortunately, wasn’t an option for critically ill COVID-19 patients who could not be easily moved to an operating room.
The alternative is a bedside procedure known as a percutaneous tracheostomy, in which tubing is inserted through a small puncture at the base of the neck—no surgery required. But even this minimally invasive innovation has raised red flags among pulmonologists because it creates aerosolized spray that can infect healthcare workers.
Enter Dr. Angel’s ingenious workaround. The dangerous spray results when doctors snake a camera down the breathing tube to guide them during the procedure. To make room for the camera, they traditionally deflate the cuff that holds the tube in place—a move that permits infectious aerosolized droplets to escape. “Instead of placing the bronchoscope inside the breathing tube, I go alongside it,” Dr. Angel explains. “That way, the cuff is always inflated and nothing is aerosolized.” This variation on percutaneous tracheostomy has been performed successfully on more than 200 patients and become the institution’s new standard of care for intubated patients.
Another example of the exceptional care NYU Langone has provided to patients with COVID-19 is the contributions of its thoracic surgeons, led by Michael Zervos, MD, chief of the thoracic surgery service at Tisch Hospital and Kimmel Pavilion, who collaborated with colleague Costas Bizekis, MD. COVID-19 can trigger a severe inflammatory response that fills the lungs with thick, tenacious secretions that often obstruct the airway, leading to oxygen deficiency. To remove these fluids, Dr. Zervos and his team have performed frequent “toilet bronchoscopies” on patients on ventilators, some intubated and others having had percutaneous tracheostomies. A bronchoscopy involves inserting a long scope into the lungs to suction out sputum, essentially unclogging them. The procedure, Dr. Zervos explains, improves oxygenation and helps prevent bacterial infections.
While bronchoscopy provides immediate and potentially lifesaving relief for patients with COVID-19, the procedure poses the threat of viral transmission to the doctors who perform it. Nevertheless, Dr. Zervos and his team accepted the risks because they believed that the benefits for patients are so vital. To lessen the potential for harm, however, they have practiced a rigorous protocol, developed with input from Robert J. Cerfolio, MD, MBA, director of clinical thoracic surgery and chief of hospital operations. “We believe they have a positive impact in outcomes,” says Dr. Zervos, “and we’ve developed a good strategy to mitigate the possibility of viral spread.”
“Dr. Angel and Dr. Zervos have had an all-in mentality,” says Mark E. Nunnally, MD, director of adult critical care services. “That level of dedication and inspiration got us through the darkest days.”