Dr. Anthony K. Frempong-Boadu combines advanced preoperative planning with extensive surgical expertise to resect a challenging spinal tumor.
Photo: NYU Langone Staff
When a patient with intensifying neuromuscular symptoms was diagnosed with an aggressive malignant tumor in a highly vascularized location, a multidisciplinary surgical team mobilized to plan a swift intervention and execute a high-risk surgery. With skilled use of advanced imaging and intraoperative technologies to support planning, the team carried out a complex strategy to safely remove the tumor and restore the patient’s function.
A Common Spinal Tumor in an Uncommon Location
With progressively worsening left-side neck pain radiating into his shoulder and upper arm for 6 months, the 72-year-old patient also began to experience progressive muscle weakness that limited his mobility. His physician suspected deltoid palsy and recommended physical therapy. When that failed to elicit improvement, MRI imaging was ordered, and this revealed a large spinal mass surrounding the patient’s left vertebral artery. At that point, the patient was referred to Anthony K. Frempong-Boadu, MD, associate professor in the Departments of Neurosurgery and Orthopedic Surgery and co-director of the Spine Center.
A biopsy revealed a chordoma—a locally aggressive primary malignant tumor with a high recurrence rate. This tumor is commonly found in the clivus and sacrum; its presentation above the sacrum in the C4 and C5 vertebral bodies, where spine compression was causing the patient’s deltoid palsy, was unusual. “These lesions look benign but behave malignantly,” notes Dr. Frempong-Boadu. “We aim to achieve the most complete resection possible to prevent recurrence, but this patient’s large tumor in the thick of the major blood vessels that feed critical brain areas made surgical intervention extremely risky and technically challenging.”
However, the tumor’s location and the patient’s progressive symptoms indicated action. As the tumor grew, it would threaten the vertebral and carotid arteries, potentially causing a catastrophic stroke or death. With the risks of both surgery and watchful waiting discussed with the patient, a wide resection and anterior reconstruction were planned.
Mapping a Delicate Anatomy for Real-Time Visualization
The site of the tumor precluded en bloc resection in favor of a more precarious intralesional resection, in order to reduce the risk of complications and achieve a better functional outcome. The approach would require a precise multidisciplinary surgical plan aided by microsurgical techniques and a cache of leading-edge technologies working together to map every inch of the delicate anatomy. “In a case like this one, you need to go into surgery with a clear plan and a realistic assessment of potential pitfalls,” notes Dr. Frempong-Boadu. “It’s like a military operation—you really need to know what your contingencies are, so you don’t get in there and realize there are land mines you didn’t expect.”
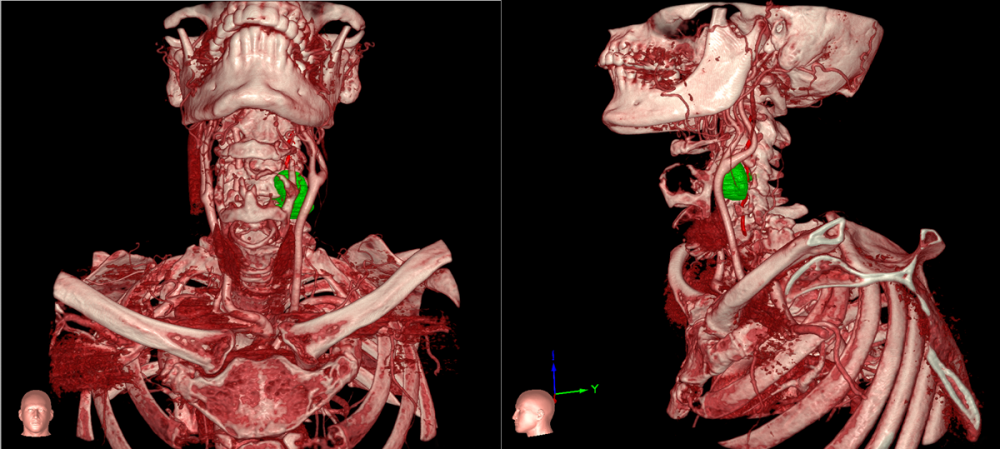
In this procedure, the greatest area of risk was in navigating the intradural and paraspinal structures, including the vertebral artery. A preoperative angiogram, performed with a Dyna spin, provided a three-dimensional view of the relationship among the tumor, bony structures, and vessels—revealing the proximity of the dominant-right and left vertebral arteries. During the surgery, Airo® intraoperative CT scanning with Brainlab computer-assisted spinal navigation would combine to inform real-time, augmented-reality navigation through Surgical Theater.
Beyond advanced technology, the carefully formulated plan relied heavily on surgical experience. For his expertise in highly technical head and neck surgery, Dr. Frempong-Boadu collaborated with Mark D. DeLacure, MD, the George E. Hall Associate Professor of Head and Neck Cancer Research in the Department of Otolaryngology—Head and Neck Surgery and associate professor in the Hansjörg Wyss Department of Plastic Surgery and Department of Neurosurgery, to perform the anterior neck dissection and subsequent approach.
“Seconds matter in these operations, so you make sure you’re prepared by having aneurysm clips in the operating room and neurointerventional radiology and surgical partners on call,” says Dr. Frempong-Boadu. “Even with the ideal multidisciplinary team in place, you need to think of everything before you get to the operating room because the stakes are just so high if you encounter complications.”
Careful Surgical Planning Circumvents Complications
With the detailed plan in place, the patient was brought to the operating room, where Surgical Theater imaging was projected onto the target anatomy and the structures drawn on his skin. With the incision planned, Dr. DeLacure performed the approach to the anterior cervical spine. The team’s careful planning expedited the identification of the tumor and proximal vessels.
Dr. Frempong-Boadu then performed a definitive resection of the anterior neck tumor, debulking the tumor using spinal navigation and microscope integration with an advanced Zeiss microscope. “The tumor was integrated into my eyepieces so I could see the outline of the tumor and achieve more precise control while working,” he notes.
After completing initial debulking of the lesion, Dr. Frempong-Boadu dissected out the left vertebral artery and removed the remaining soft tissue neck component of the tumor around the artery, aided by the Airo® CT scan. “Fortunately, when we picked up the vessel it turned out there was a nice capsule between the vessel and the tumor providing some leeway, and we took our time in removing the tumor from around it,” he says.
With the anterior tumor resected, Dr. Frempong-Boadu turned his attention to resecting fractured vertebrae and the epidural tumor and performing the anterior spinal reconstruction. The patient was then turned for posterior reconstruction, including a posterolateral fusion of C3–C6. A repeat intraoperative CT scan confirmed both complete resection and excellent anteroposterior cervical reconstruction and hardware placement, and the patient was taken to recovery.
Experience, Intraoperative Tools Combine for Positive Outcome
With the surgery successfully completed, the patient began the work of regaining function. He spent time postoperatively as an inpatient at Rusk Rehabilitation to receive physical and occupational therapy to support his independence during recovery. He reported symptom relief immediately after surgery and ambulated readily. Though he experienced some weakness over the course of proton beam therapy, used adjuvantly to reduce recurrence risk, he has experienced gradual recovery from his left deltoid weakness and continues to gain strength.
In addition to the benefits of careful preoperative planning, surgical expertise played a pivotal role in delivering a positive outcome for this patient despite a high-risk tumor in a challenging location. “When structures are disrupted by a tumor, the challenging aspect of surgery is to determine where you are and what you are seeing—to have that anatomy imprinted in your head,” says Dr. Frempong-Boadu. “My training in trauma and tumors taught me to find a normal structure, then work backward toward abnormal, so in this case I was able to visually resect the tumor from experience and confirm success with technology.”